Patterns of failure in oral cavity squamous cell carcinoma treated with adjuvant radiotherapy
OC-0432
Abstract
Patterns of failure in oral cavity squamous cell carcinoma treated with adjuvant radiotherapy
Authors: AVIPSA DAS1, INDRANIL MALLICK2, SANJOY CHATTERJEE2
1Princess Margaret Cancer Center, Radiation Oncology, TORONTO, Canada; 2TATA MEDICAL CENTER, CLINICAL ONCOLOGY, KOLKATA, India
Show Affiliations
Hide Affiliations
Purpose or Objective
Adjuvant radiotherapy (RT) is the standard of practice in patients with histopathological high risk factors post surgical resection in oral cavity squamous cell cancer (OCSCC). There is limited data to guide the post-operative target volumes, especially treatment of ipsilateral/ contralateral neck. We report our institutional data of OCSCC patients treated with adjuvant radiotherapy, focusing on the incidence and predictors of local, nodal and distant failure.
Material and Methods
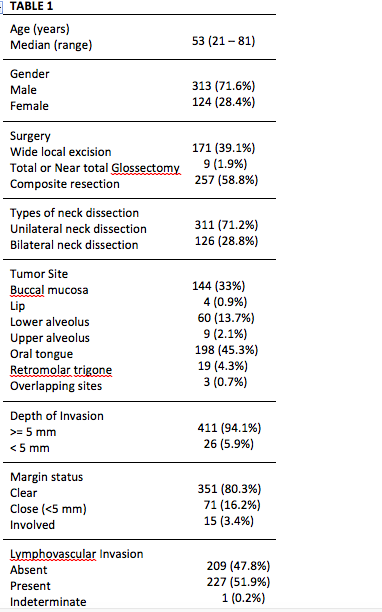
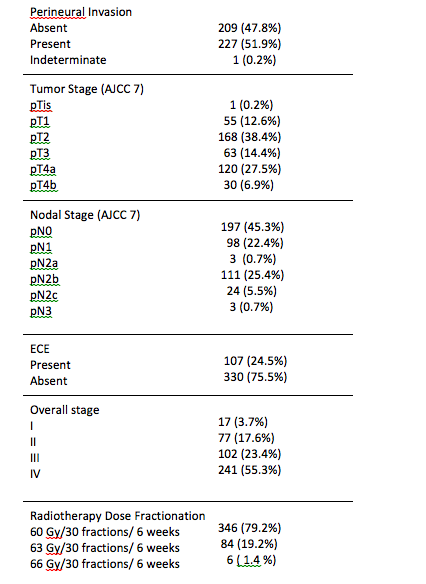
Details of patients between August 2011 to July 2016, were retrieved from our prospectively maintained electronic database. Adjuvant RT was delivered in all patients with pT3/T4 tumor, close margins, node-positive, and extracapsular extension. Patients with more than two intermediate risk factors (lymphovascular invasion, perineural invasion (PNI), depth of invasion >=5mm, poor tumor differentiation status, and tongue primary) were being offered adjuvant RT, from 2015. Concurrent chemotherapy was administered to patients with extracapsular extension and involved/ very close margins. Re-staging PET-CT was done in patients with evidence of recurrence.
Overall survival, local control, nodal and distant metastases free survival were defined from the date of registration to date of death from any cause, local recurrence, or appearance of new nodal or distant metastases, respectively.
Results
A total of 437 patients were identified from our database. The median duration of follow up was 39 months. A majority of node negative (pN0) patients (89%; 176/198) received RT to the ipsilateral neck. Amongst 239 pathologically node positive patients, 140 (32%) received RT to bilateral neck. At 3 years, the probability of local control, nodal control, freedom from distant metastasis, disease-free survival and overall survival was 84%, 87%, 85%, 70% and 82.3%, respectively. Local control at 3 years was better for clear/ close margins vs involved margins (85% vs 67%; p 0.04). Forty nine (11.2%) patients had nodal recurrences. Nodal control (NC) at 3 years correlated to nodal stage (N0 94% > N1 84% > N2 79%> N3 64%; p 0.001); NC was better for ECE neg vs ECE pos ( 91% vs 74%; p <0.001), and for PNI negative vs. PNI positive primaries (91.3% VS 83.4%; p 0.04). Distant metastases were recorded in 54 (12.4%) patients. Distant control was associated with nodal stage (N1>N2>N3; p<0.001), and was better with ECE negative vs ECE positive patients (p<0.001).
Conclusion
This is one of the largest series looking into the patterns of failure across all risk groups of OCSCC patients. Margin status independently predicted local outcomes, whereas higher nodal stage and extracapsular extension correlated to nodal and distant failures. The incidence of any contralateral failure or ipsilateral level IV failure was low and independent of inclusion into target volumes.