External validation of NTCP models for dysphagia and xerostomia in the elderly patients with HNSCC
Linda Sommers,
The Netherlands
OC-0436
Abstract
External validation of NTCP models for dysphagia and xerostomia in the elderly patients with HNSCC
Authors: Linda Sommers1, Hans Paul van der Laan1, Lisa van den Bosch1, Johanna van den Hoek1, Tineke van Zon-Meijer1, Edwin Oldehinkel1, Hans Verbeek1, Gyorgy Halmos2, Roel Steenbakkers1, Johannes Langendijk1
1University Medical Centre Groningen, Radiation Oncology, Groningen, The Netherlands; 2University Medical Centre Groningen, Otorhinolaryngology/Head & Neck Surgery, Groningen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
We recently reported on a comprehensive individual toxicity risk (CITOR) profile, including normal tissue complication probability (NTCP) models for toxicities after radiotherapy for head and neck squamous cell carcinoma (HNSCC). It has often been assumed that elderly patients (age ≥ 70 years) are generally more susceptible to radiation-induced toxicities. Therefore, this study aimed to externally validate these models in a cohort of elderly HNSCC patients.
Material and Methods
Prospectively collected data of all consecutive elderly patients with HNSCC treated with definitive RT from April 2007 to July 2020 were analysed.
Toxicity outcomes consisted of 4 dichotomised outcomes: CTCAEv4.0 physician-rated dysphagia ≥ Grade 2; dysphagia ≥ Grade 3; EORTC QLQ-H&N35 patient-rated moderate-to-severe xerostomia and severe xerostomia. The NTCP-models for dysphagia at 6, 12, 18 and 24 months after RT included the mean dose to the oral cavity and the pharyngeal constrictor muscles, baseline dysphagia, and primary tumour site as predictors
The NTCP-models for late xerostomia (same time points) included the mean dose to the parotid and submandibular glands and baseline xerostomia as predictors.
The original NTCP-models after RT treatment were externally validated in a general HNSCC population. Discrimination (ROC-AUC) and calibration among elderly patients were evaluated, and appropriate model updates were done when needed.
Results
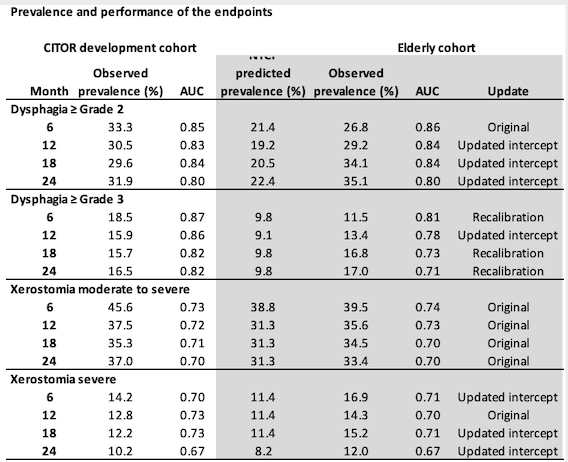
The study population consisted of 310 elderly (29.6%) of the total HNSCC population of 1047 patients. Compared to the development cohort, the prevalence of dysphagia increased with time in the elderly cohort, with a lower prevalence at six months and a higher prevalence at 24 months (Table 1). Models developed for dysphagia ≥Grade 2 had high discrimination in the elderly cohort (AUC: 0.80-0.85) but required an update of the intercept as the observed prevalences were higher than predicted. Models for dysphagia ≥ Grade 3 showed lower discrimination (AUC: 0.71-0.81) and needed recalibration for most time points for use in elderly patients. The original models for moderate-to-severe xerostomia performed well, and no model adjustments were required. For severe xerostomia, the prevalence was higher than predicted, requiring an adjustment of the intercept. These adjusted models showed comparable discrimination (AUC: 0.67-0.71) as in the original models.
Conclusion
The CITOR NTCP-models perform reasonably well in elderly patients. The original NTCP-models for dysphagia ≥Grade 2 and xerostomia could be used, with an updated intercept for some time points due to the higher observed rates than predicted. Model adjustment was also needed for the dysphagia ≥ Grade 3 NTCP-models, suggesting higher susceptibility in elderly patients for this side effect.