Tumor Control Probability following Radiosurgery of Brain Metastases With and Without Retreatment
OC-0459
Abstract
Tumor Control Probability following Radiosurgery of Brain Metastases With and Without Retreatment
Authors: Manju Sharma1, Michael T Milano2, Michael Cummings2, Isaam El Naqa3
1UCSF, Radiation Oncology, San Francisco, USA; 2University of Rochester Medical Center, Radiation Oncology, Rochester, USA; 3Moffitt Cancer Center, Radiation Oncology, Florida, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Tumor control probability (TCP) models were developed to quantify the relationship between radiation dose and local control after single-fraction stereotactic radiosurgery (SRS) for brain metastasis with and without retreatment.
Material and Methods
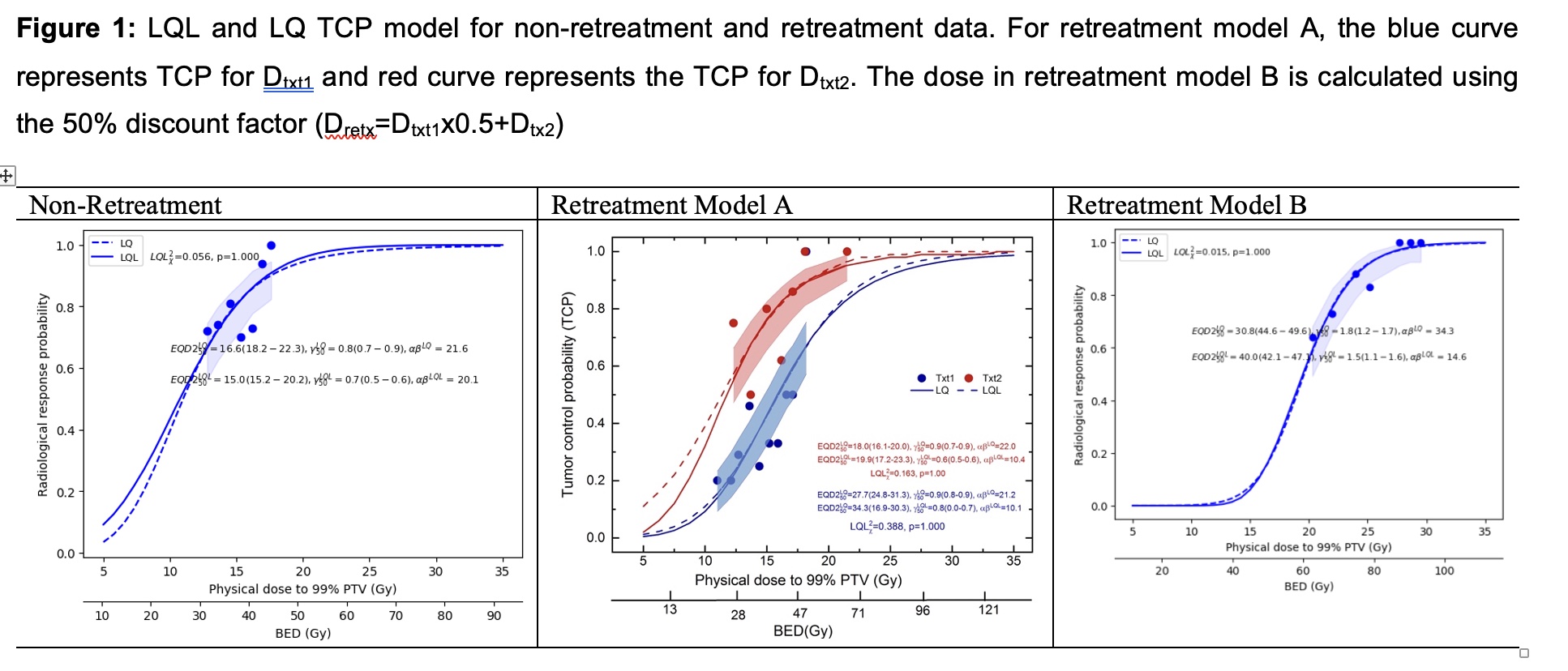
Patients treated with single-fraction LINAC-based SRS at a single institution from 2003-2016 were used to model TCP. The non-retreatment cohort included 173 patients with 493 metastatic lesions while the retreatment cohort included 25 patients with 50 metastatic lesions. For retreatment, the patients were usually prescribed the same tumor dose irrespective of the dose received in the initial treatment. Following the recent HyTEC methodology the dose to 99% of each lesion’s planning-target-volume (D99) and at one-year follow-up were fitted using the linear-quadratic (LQ) and linear-quadratic-linear (LQL) model-based dose conversions to correct for the dose per fraction effect. LQ and LQL models were fitted for non-retreatment lesions. For the retreatment dataset, two different methods were used: (A) Two separate LQ and LQL TCP models for initial (Dtxt1) and second treatment (Dtxt2) (4 models total); (B) one set of LQ and LQL models for retreatment dose with a correction factor of 50%, i.e., Dretx=Dtxt1x0.5 + Dtx2 (2 models total). Model A is based on the common clinical practice for retreatment of brain metastases. The quality of fit was assessed using Chi-2.
Results
The LQ and LQL models fitted well with the non-retreatment and retreatment lesion data (LQL Chi-2= 0.015-0.388, p=1.0). For our non-retreatment patient data, the fitted EQD2_50, a/b and gamma50 values were close to HyTEC multi-institution modeling results and the 1-year TCP was estimated at 90% for a D99 of 17.6Gy. Keeping the same 90% TCP, relatively higher D99 (24.5Gy) was predicted for the retreatment model B. Interestingly, in model A, the predicted 90% TCP at D99 for retreatment (Dtxt2) was lower than the initial (Dtxt1) 18.5Gy vs 23.3Gy. The mean fitted LQL EQD2_50 for non-retreatment and re-treatment model A and B, respectively were 15Gy, 39.3Gy (Dtx1), 19.9Gy (Dtx2) and 40.3Gy (Dretx).
Conclusion
For our patient cohort treated with SRS for brain metastases, the non-retreatment TCP model fitting parameters were in a close approximation to the recent HyTEC brain SRS publication based on pooled data from published studies. This is an effort to understand the TCP in SRS for retreatment of brain metastases. For the 90% TCP in retreatment lesions, using model A, we observed lower D99 for the second treatment. These unanticipated results highlight possible tumor sensitivity to radiation during re-treatment. Further validation needs to be done on a larger dataset.