Minimising radical radiotherapy commencement time for lung cancer to improve clinical outcomes
Minal Padden-Modi,
United Kingdom
PD-0670
Abstract
Minimising radical radiotherapy commencement time for lung cancer to improve clinical outcomes
Authors: Minal Padden-Modi1, Joyce Cheng1, Rachel Kirby1, Nicola Twyman1, Shahzeena Aslam1, Venkata Ramesh Bulusu1, David Gilligan1, Alexander Martin1, Nisarg Pipalia1, Anna Maria Shiarli1, Huiqi Yang1, Kamalram Thippu Jayaprakash1
1Cambridge University Hospitals NHS Foundation Trust, Clinical Oncology, Cambridge, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
The UK National Optimal Lung Cancer Pathway (NOLCP) provides guidance to improve and streamline the treatment pathway for lung cancer1. An increased time to treatment is independently associated with poorer survival in non-small cell lung cancer2 (and also likely in small cell lung cancer). This work reviews radical radiotherapy (RT) commencement times in a tertiary UK referral centre, identifying opportunities to shorten the pathway for patients with lung cancer.
Material and Methods
Patients treated with radical (chemo-) RT from April-October 2020 were identified. Data on various time points between referral and treatment were collected from electronic patient records and analysed. LEAN methodology was applied for root-cause analysis to identify patients receiving delayed treatment and to consider actions to improve treatment start times.
Results
n = 77 (SABR - 22, concurrent chemo-RT - 20, RT alone/sequential chemo-RT - 26). Overall median time from referral to treatment (in days): all patients - 27; SABR - 27; concurrent chemo-RT - 32; RT alone/sequential chemo-RT - 26. Individual median time-frames (in days) for all patients: RT referral to CT (7); CT to contouring [image segmentation] (6); contouring to physics planning (2); physics planning to checking (3); physics checking to delivery quality assurance [DQA] (1); DQA to commencement of RT (5). Respective time frames for the different treatment subgroups are shown below (Figure 1).
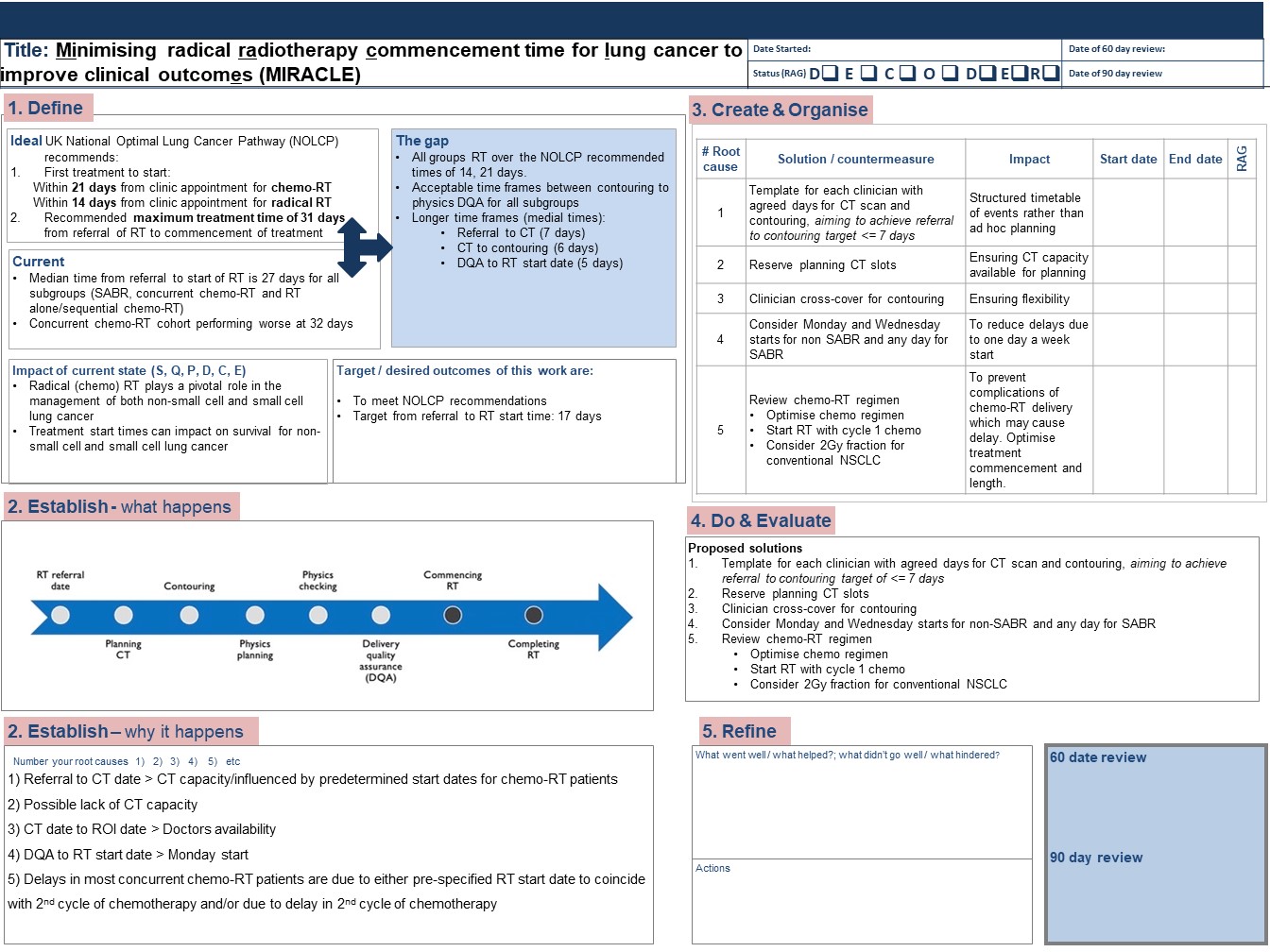
Root-cause analysis identified areas for improvement including organisation of planning CT, contouring and DQA, and the following solutions were agreed (Figure 2).
● A clinician-specific timetable for referral to contouring with a target of ≤ 7 days.
● Dedicated planning CT slots for radical lung RT patients.
● Ensuring clinician availability by arranging cross cover for contouring within the lung RT team.
● RT to start on Monday and Wednesday for non-SABR and any day for SABR.
● Optimise chemotherapy regimens to ensure on time delivery of chemo-RT.
Figure 1
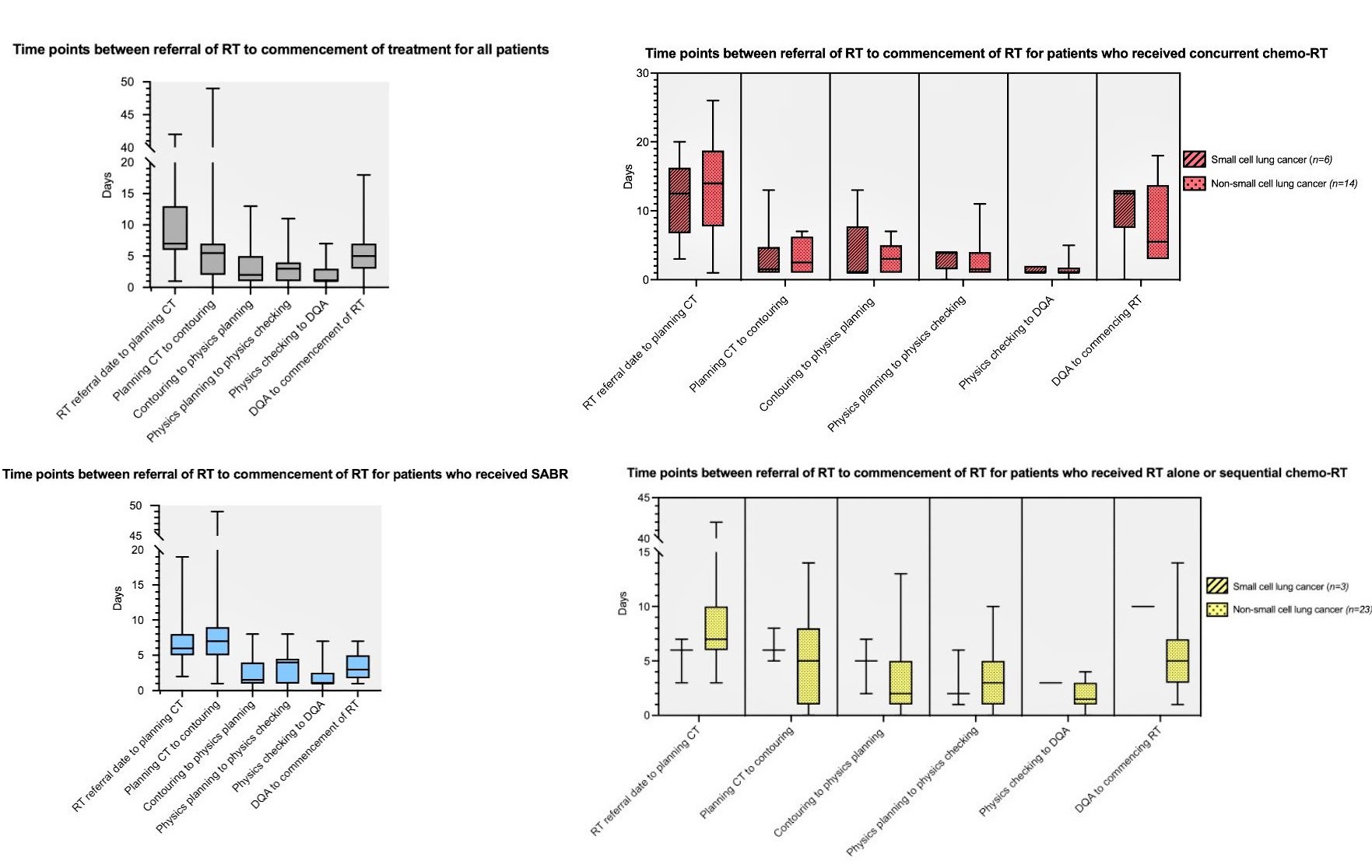
Figure 2
Conclusion
Our work demonstrated current performance and identified areas for improvement within the radical lung RT pathway. Following implementation of the recommended changes, follow up work is planned to evaluate their impact.
References
1Lung Clinical Expert Group NHS England. National Optimal Lung Cancer Pathway; 2020.
2Taylor R. et al. The Effects of Time to Treatment Initiation for Patients With Non–small-cell Lung Cancer in the United States; Clinical Lung Cancer; 2020.