Introduction of IMPT for NSCLC patients: the learning curve in practice.
Robin Wijsman,
The Netherlands
PD-0667
Abstract
Introduction of IMPT for NSCLC patients: the learning curve in practice.
Authors: Robin Wijsman1, Olga Chouvalova1, Petra Klinker1, Anne Niezink1, Annija Van der Leest1, Fred Ubbels1, Marleen Woltman-van Iersel1, Stefan Both1, Erik Korevaar1, Johannes Langendijk1
1University Medical Center Groningen, Radiation Oncology, Groningen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
In October 2019, we started to treat NSCLC patients with intensity
modulated proton radiotherapy (IMPT). We planned to initiate a dose escalation
RCT, but we felt that this should only start beyond the steepest part of the
learning curve. Therefore, the objective of this study was to explore our
learning curve in terms of treatment planning and delivery.
Material and Methods
The model-based approach was used to select patients for IMPT. Model-based
selection (IMPT compared to VMAT) was based on 2 NTCP-models (Grade ≥2 acute
esophageal toxicity (AET) and Grade ≥2 radiation pneumonitis (RP)) and one
prediction model for 2-year mortality (2yM). All patients received
(chemo)radiation (25x2.4 Gy) for NSCLC. Robust IMPT plans were created using
typically three beams and a 3D robustly optimized planning technique (5 times
layered rescanning). Initially, maximum target motion allowed for IMPT was 10
mm, from March 2020 on this was extended to 15 mm. Online position verification
consisted of daily (consecutive) body surface scanning, 2D kV imaging and
cone-beam CT imaging. Weekly repeated (4D) CTs were acquired; the treatment
plan was adapted in case of inadequate target coverage visualized on the repeated
CT. The following characteristics were evaluated: ΔDose
(mean doses for heart, lungs and esophagus) and ΔNTCP (for AET, RP and 2yM), all
based on the nominal treatment plan. Treatment delivery times at the gantry and
the number of plan adaptations were evaluated also. To evaluate the learning
curve, the cohort was split in two: Cohort A ranged from October 2019 to March
31st 2020 (n=24), Cohort B ranged from April 2020 to September 2021
(n=90).
Results
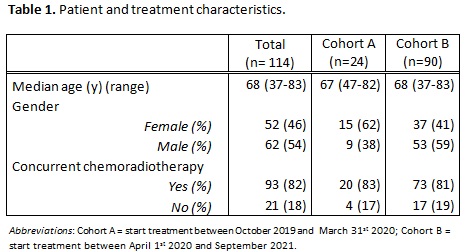
For patient and treatment characteristics, see Table 1. After
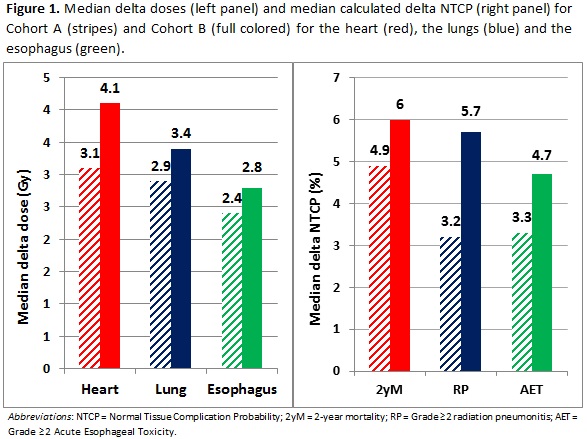
radiotherapy plan comparison (IMPT vs VMAT), the median ΔDose (mean) for heart
(3.1 Gy vs 4.2 Gy, p=0.087), lung
(2.9 Gy vs 3.4 Gy, p=0.13) and
esophagus (2.4 Gy vs 2.8 Gy, p=0.48)
was larger in Cohort B compared to Cohort A. Median ∆NTCP increased in Cohort B
compared to Cohort A: from 4.9% to 6.0% (2yM, p=0.26), 3.2% to 5.7% (RP, p=0.06)
and 3.3% to 4.7% (AET, p=0.49), respectively (figure 1). Treatment delivery times decreased from an
average of 34 minutes (Cohort A) to 25 minutes (Cohort B). Eleven (46%) of the treatment
plans in Cohort A needed adaptation, compared to 20 (22%) in Cohort B.
Distribution of the timing of these plan adaptations were equally balanced over
the radiotherapy course and were similar for both cohorts. Comparing the first
half of Cohort B with the second half of Cohort B: ΔDose, ∆NTCP and treatment
delivery parameters were similar for both groups.
Conclusion
The
observed increase in ΔDose
and
ΔNTCP,
and
more efficient treatment delivery over time indicates that a learning curve was
present after the introduction of IMPT. Awareness of the learning curve is
important in further optimizing treatment. This may have implications for the
initiation of clinical studies while still on the steep part of the learning
curve.