Validation of the interaction between peritumour density and dose for local relapse in lung SABR
PD-0673
Abstract
Validation of the interaction between peritumour density and dose for local relapse in lung SABR
Authors: Angela Davey1, Maria Thor2, Marcel van Herk1, Corinne Faivre-Finn1, Joseph O Deasy2, Andreas Rimner3, Alan McWilliam1
1The University of Manchester, Division of Cancer Sciences, Faculty of Biology, Medicine and Health, Manchester, United Kingdom; 2Memorial Sloan Kettering Cancer Center, Medical Physics, New York, USA; 3Memorial Sloan Kettering Cancer Center, Radiation Oncology, New York, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Local relapse (LR) can occur after lung SABR due to inadequate coverage of microscopic disease (MDE). A Cox-per-radius method has been applied to study the interaction between CT biomarkers that predict MDE and incidental dose, with preliminary data reported at ESTRO 2021. The resulting model proposed high peritumour density combined with high dose standard deviation (SD) outside the GTV as a predictor of LR. We update and explore the model in internal training and external validation cohorts.
Material and Methods
275 early-stage NSCLC patients treated to 60Gy (199, internal training data) or 50Gy (76, external validation data) in 5 fractions were collated from two institutions. In both, dose distributions were accumulated for respiratory motion and converted to EQD2. A pre-analysis plan was registered.
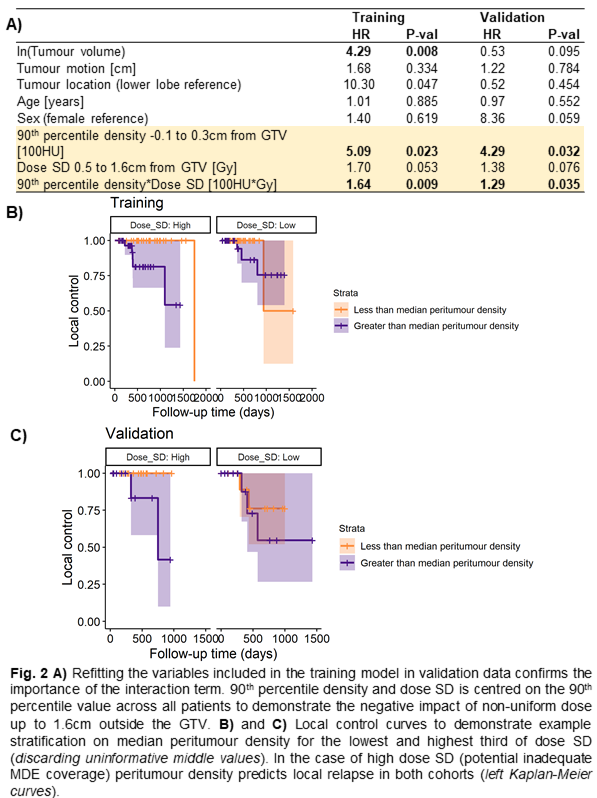
Cox-per-radius was implemented to build a map of the interaction between 90th percentile density and dose SD in independent 1mm annuli outside the GTV, with a multiple-testing correction on region size implemented. Density and dose were averaged in annuli defined by the map and included in a Cox model. Bootstrapping was performed with 500 resamples to test stability and improvement in c-index compared to clinical variables after adjusting for optimism.
For external validation, the overall models (clinical, including dose and density, and including the interaction) were explored with and without re-fitting in the external data.
Results
Cox-per-radius detected one region (at the GTV edge for density and 1 cm outside the GTV for dose) involved in LR (Fig. 1A). Only the model including the interaction improved the clinical model after bootstrapping on the internal dataset (Fig. 1B). The models did not directly translate when validating on the external dataset due to difference in demographics (Fig. 1C), prescription, and contouring (judged qualitatively). Model coefficients were, therefore, re-fitted, establishing the importance of the interaction in both datasets.
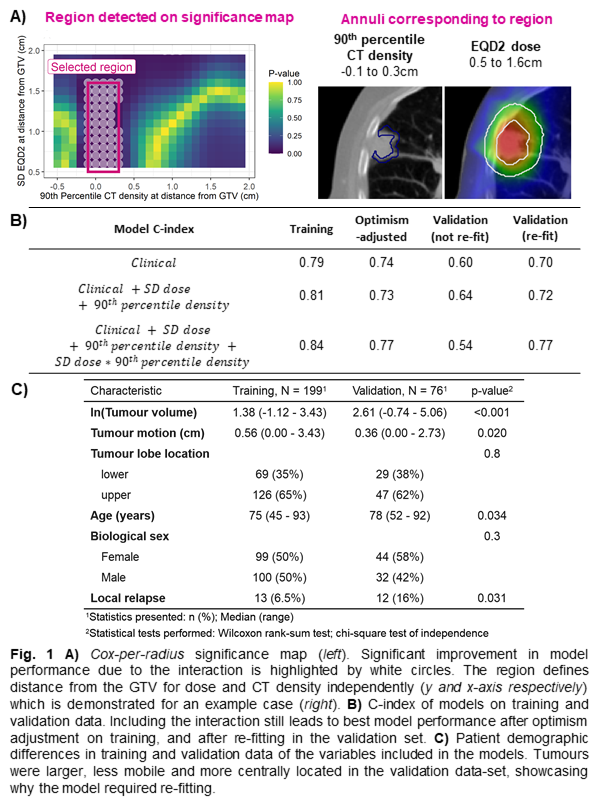
In Figure 2A, hazard ratios are reported at the 90th percentile of SD dose and peritumour density across patients, as hazard can only be interpreted at specified values of the interacting variable. The result demonstrates that higher density is associated with risk of LR for non-uniform dose outside the GTV. The dose required to this region (Fig. 1A) is not yet known, but example stratification is shown (Fig. 2B and C). Dose SD outside the GTV only weakly correlates with tumour dose, and instead reflects PTV heterogeneity and sharp dose fall-off (data not shown).
Conclusion
This study confirmed an interaction between peritumour density and incidental dose that predicts LR regardless of cohort differences. We validated that LR risk can be stratified on peritumour density and is increased for patients with non-uniform dose outside the GTV. To avoid LR, dose up to 1.6cm outside the GTV should be increased for patients with high peritumour density by larger margins or constraints on PTV heterogeneity to reduce sharpness of dose fall-off.