Cardiac toxicity predicts mortality in NSCLC patients: interim analysis of the LUNG-HEART Study
PD-0672
Abstract
Cardiac toxicity predicts mortality in NSCLC patients: interim analysis of the LUNG-HEART Study
Authors: Marzia Cerrato1, Serena Badellino1, Fabio Menegatti1, Ilaria Bonavero1, Cristiano Grossi1, Bruna Lo Zito1, Erika Orlandi1, Alessio Gastino1, Erica Maria Cuffini1, Ludovica Blasi1, Cristina Mantovani1, Ramona Parise1, Umberto Ricardi1, Mario Levis1
1University of Torino, Department of Oncology, Torino, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
To date no consistent dosimetric parameters related to overall survival
(OS) and cardiac toxicity in early stage (ES) and locally advanced (LA) NSCLC
patients have been identified. The aim of this prospective study is to
investigate for any existing correlation between the dose delivered to the
heart and to cardiac and vascular structures and OS, non-tumor-related survival
and the development of cardiac toxicity, in ES-NSCLC and LA-NSCLC patients
treated with definitive RT.
Material and Methods
Patients with PS ECOG score 0-1 and no previous RT treatment to the
mediastinum were included. Details on pre-existing cardiovascular risk factors and comorbidities, ongoing drug therapies
and lung function tests were collected at baseline. The Charlson
Comorbidity Index (CCI) was calculated at the time of the first clinical
evaluation. Cardiac substructures (valves, chambers and coronary arteries) were
prospectively contoured in order to collect dosimetric data. Cardiac toxicity events were evaluated with
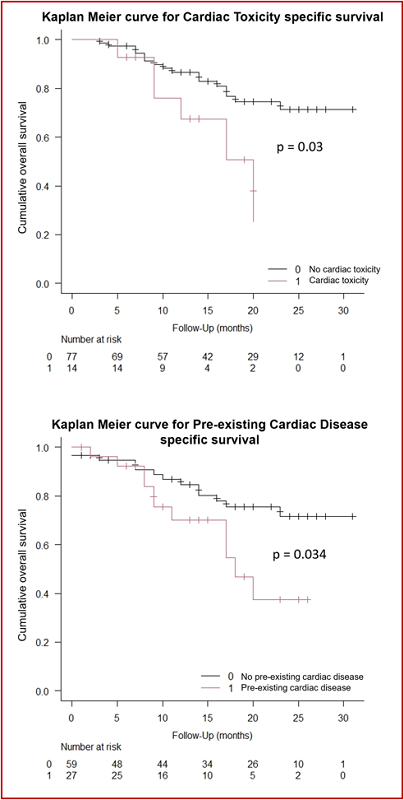
the CTCAE 5.0 grading. OS was estimated with the Kaplan-Meier method from
the date of the last of RT session.
Results
From March 2019 to
September 2021, 115 patients were enrolled. Of these, 69 received Stereotactic Ablative
RT (SABR) with a “risk adapted” fractionation schedule (1-8 fractions); 46
LA-NSCLC patients were treated with combined chemo-radiotherapy, with doses of 54-60
Gy (2 Gy/fr). Overall, 14 patients (15%) developed at least one event of
cardiac toxicity during the observation period and 26 patients were dead (16
ES-NSCLC and 10 LA-NSCLC) at the time of this analysis. With a median follow up
of 14 months, we observed that patients who developed cardiac toxicity had a
higher risk of death at 1 year compared to the others (1yOS: 67.5 % vs 86.5 %,
p= 0.03). Moreover, the presence of pre-existing cardiac diseases had a
negative impact on OS at 1 year (70% vs 84.7% p=0.034) (Figure 1).
Hazard ratios for pre-existing cardiac diseases and cardiac toxicity were 2.33
[IC95%=1.036-5.253] and 2.71 [IC95%=1.044-7.05], respectively. No correlation
between the CCI (0-4 vs ≥5) and OS was revealed (p= 0.77) on the overall
population. The analysis of dosimetric parameters was carried out separately
for the two groups. Despite the limitations due to our modest sample size, heart V40
and V50 were associated with cardiac toxicity in the LA-NSCLC group, with an OR
of 1.46 (p=0.043) and 1.61 (p=0.05), respectively. To date no correlations were
found in the ES-NSCLC group.
Conclusion
According to our results, pre-existing heart
comorbidities and the onset of cardiac toxicity predict a higher risk of
mortality in NSCLC patients treated with RT. Therefore, the risk of developing
cardiac toxicity must be carefully considered in all patients. Preliminary
dosimetric data suggest a possible correlation between heart dosimetry and the
development of RT related cardiac toxicity, but longer follow up periods are
required to confirm these findings.