Comparison of synthetic CT generation methods for MRI-only definitive pelvic radiotherapy
Laura O'Connor,
Australia
PD-0321
Abstract
Comparison of synthetic CT generation methods for MRI-only definitive pelvic radiotherapy
Authors: Laura O'Connor1,2, Jae Hyuk Choi3,1, Jason Dowling4, Helen Warren-Forward2, Jarad Martin5,6, Peter Greer1,3
1Calvary Mater Hospital, Radiation Oncology, Newcastle, Australia; 2University of Newcastle, School Health Sciences, Newcastle, Australia; 3University of Newcastle, School of Mathematical and Physical Sciences, Newcastle, Australia; 4Commonwealth Scientific and Industrial Research Organisation (CSIRO), Australian E-Health Research Centre, Herston, Australia; 5Calvary Mater Newcastle, Radiation Oncology, Newcastle, Australia; 6University of Newcastle, School of Medicine and Public Health, Newcastle, Australia
Show Affiliations
Hide Affiliations
Purpose or Objective
There are several means of synthetic computed tomography (sCT)
generation for MRI-only planning in the
literature. The aim of this research was to apply four of the most popular
methods of sCT creation to facilitate MRI only radiation therapy treatment
planning for male and female rectum, anal canal, cervix and endometrium
neoplasms. The sCT methods were validated against conventional CT, with regards to Hounsfield unit (HU) estimation and plan
dosimetry.
Material and Methods
Paired MRI and CT scans of forty patients, treated for a range of pelvic
malignancies were used for sCT generation and validation. Bulk density
assignment, tissue class segmentation, hybrid atlas and deep learning sCT
generation methods were applied to all 40 patients. Each sCT creation method
used was based on successfully applied methods in the literature. Dosimetric
accuracy was assessed by dose difference at reference point, dose volume
histogram (DVH) parameters and 3D gamma dose comparison. Due to the
non-parametric nature of the data, statistical significance was determined
using a Mann-Whitney U-test with a significance level of 0.05. Hounsfield unit
estimation was assessed by mean error and mean absolute error in HU value
between each sCT and CT.
Results
There was no statistically significant dose difference to CT at the ICRU
reference point for any of the sCT methods (Table 1). The median percentage dose difference between the CT and sCT was <1.0% for all sCT methods, with the lowest median percentage dose difference for the deep learning method at -0.03% (Interquartile Range (IQR) 0.13, -0.31) and the largest difference for the bulk density assignment at -0.73% (IQR -0.10, -1.01). The median DVH dose difference for all structures and parameters combined was less than 0.5% for all sCT methods (Figure 1).
Table 1 ICRU median percentage dose
difference and median DVH dose difference by sCT method
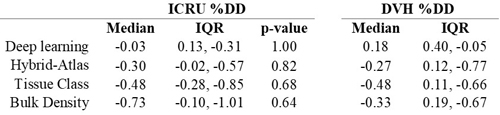
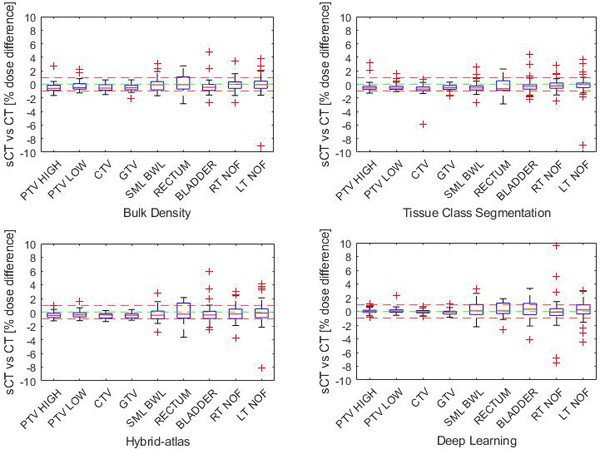
Figure 1 Percentage DVH dose difference by structure (each structure
parameters combined) for each synthetic CT method.
The mean 3D gamma dose
agreement at 3%/2mm amongst all sCT methods was 99.8%. The highest agreement at
1%/1mm was 97.3% for the deep learning method and lowest was 93.6% for the bulk
density method. The deep learning and hybrid atlas techniques gave the lowest
difference to CT in mean error and mean absolute error in HU estimation for the
whole body, bone and soft tissue estimations, reflecting the dosimetric
results.
Conclusion
Bulk density assignment, tissue class segmentation, hybrid-atlas and
deep learning methods of sCT generation all result in similarly high dosimetric
agreement for MRI only planning of male and female cancers of the rectum, anal
canal, cervix and endometrium. Choice of sCT generation technique can be guided
by department resources available and image guidance considerations, with
minimal impact on dosimetric accuracy