Reproducibility of deep inspiration breath hold during RT for lung cancer patients.
Anne-Mette Bang Rasmussen,
Denmark
PD-0653
Abstract
Reproducibility of deep inspiration breath hold during RT for lung cancer patients.
Authors: Anne-Mette Bang Rasmussen1, Ditte Sloth Møller1, Lone Hoffmann1, Marianne Marquard Knap1, Hjørdis Schmidt1, Mai Lykkegaard Ehmsen1, Thomas Ravkilde1, Esben Worm1, Margit Holst Andersen1
1Aarhus University Hospital, Department of Oncology, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Deep Inspiration Breath
Hold (DIBH) during RT for lung cancer (LC) patients is attractive, as it may
reduce dose to the lungs and heart compared to free breathing RT. However, geometric
instability during several breath holds may decrease the target coverage. In this study, we investigate the
reproducibility of DIBH during treatment planning and delivery.
Material and Methods
Twenty-four LC patients were treated with
DIBH-RT. The RPM system (Varian, CA) with an external marker (EM) placed
caudally on the thoracic cage was used as a surrogate for the DIBH level. The
patients were trained in performing DIBH before planning CT (pCT) and at the
first three treatments. For all scans and treatments, the DIBH level measured
by EM was ≤2mm. Four DIBH pCT scans were acquired: one for RT planning and
three to assess the positional difference between DIBHs (inter-DIBH) and this
uncertainty was included in the margin. To assess inter-DIBH uncertainty during
treatment, we acquired
and compared pre-treatment CBCT scans for daily setup on the tumour (CBCT1) and
post-treatment CBCT scans (CBCT2) at the first three fractions and once a week
afterwards.
Results
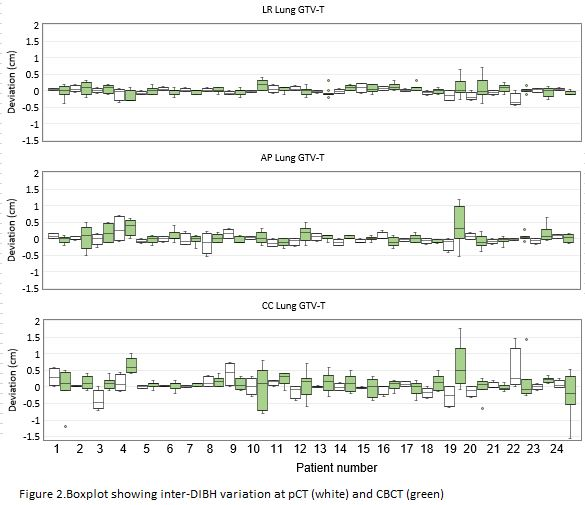
In Fig.1 left,
the inter-DIBH uncertainty between the four repeated pCTs is shown for one lung
cancer patients. Fig. 1 right shows the inter-DIBH uncertainty between CBCT1
and CBCT2 for one fraction for the same patients. A much larger difference is seen for CBCT scans
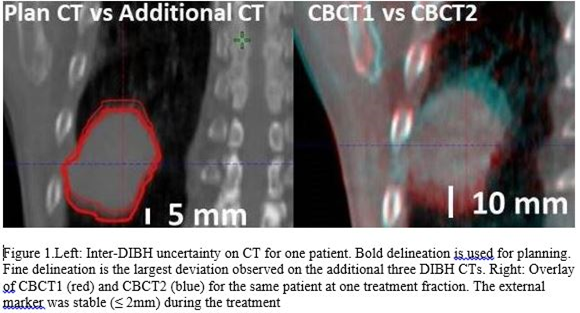
for the selected patient. This is the case for most of the LC patients, as seen
in the boxplot for the primary tumour (GTV-T) in Fig. 2. For 67% of LC patients, larger variation was seen at
CBCT in the CC direction. For all patients, the median [range] inter-DIBH
motion in LR, AP and CC was 1mm [1-5], 2mm [1-8], and 3mm[0-15] at pCT and 3mm
[1-11], 3mm [1-18], and 6mm [1-21] at CBCT, respectively. Our experience is
that a proper introduction to DIBH is crucial for a high level of patient
compliance. This includes showing the patient the impact
of how the EM moves, when the breath is hold multiple times, and what happens
when e.g. the EM is brought into position based on lifting the lower back
instead of the thoracic wall. Also ,the difference between abdominal and
thoracic DIBH should be discussed. Based on this, a checklist was developed for
the radiographers in order to document how the patient performs DIBH during pCT
and the RTT´s uses the checklist while training the patient before start of
treatment. Likewise, it seems to be important that patients know that if the
DIBH is becoming exhausting they can just breath out and take a break.
Conclusion
Inter-DIBH uncertainties
vary a lot between patients. For some patients, the size of the uncertainties
will undermine the advantages of DIBH. DIBH-pCTs acquired before treatment do
not predict the inter-DIBH uncertainty observed during treatment. Proper
training of the patient is important to ensure reproducible DIBH.