A comparative analysis of two fractionation protocol of simultaneous integrated boost-IMRT for LAHNC
PO-1213
Abstract
A comparative analysis of two fractionation protocol of simultaneous integrated boost-IMRT for LAHNC
Authors: Pragya Singh1, Deepa Joseph2, Sweety Gupta2, Debanjan Sikdar2, Ajay S Krishnan3, Abhishek Chakravarty2, Nidhi Sharma2, Arvind Diundi2, Prof Manoj Gupta2
1All India Institute of Medical Sciences, Radiation Oncology , Rishikesh, India; 2AIIMS Rishikesh, Radiation Oncology, Rishikesh, India; 3TMH Varanasi, Radiation Oncology, Varanasi, India
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiation therapy for locally advanced squamous cell carcinoma of the head and neck (LAHNC) has changed considerably over the last few years with the advancement of intensity modulated radiation therapy (IMRT) and the use of an altered fractionation schedule. With the advent of simultaneous accelerated boost IMRT (SIB-IMRT), we have achieved an acceptable toxicity profile with less time for treatment completion. Worldwide, different protocols for SIB-IMRT are used, which have a comparable outcome to the already established Sequential Boost IMRT. Till date, there has been no comparative study of two different SIB-IMRT protocols with different dose fractionation and time comparing toxicity and outcome. In our institute, we are planning to compare the acute toxicity profile and disease outcome of two different SIB-IMRT protocols which have already been established individually.
Material and Methods
We performed a retrospective data review of patients with locally advanced head and neck cancer who received definitive concurrent chemo-radiotherapy with either of these SIB-IMRT protocols consisting of radiation with 66 Gy in 30 fractions (Group A) or 69.96 Gy in 33 fractions (Group B) between April 2018 and February 2022. Eligibility included histopathology-proven AJCC Stage III-IVB squamous cell carcinoma of the oropharynx, hypopharynx, and larynx in which curative surgical resection was not indicated or recommended. Patients were at least 18 years old with an Eastern Cooperative Oncology Group (ECOG) performance status of 0–2. We excluded patients with a history of previous or concurrent malignancy or metastatic disease. Data on the patient profile, tumour profile, and treatment history were collected and analysed. The minimum follow-up period considered was 9 months. Local control at 3 months and 6 months as well as overall survival were assessed. The Chi square test was used for comparing qualitative data, whereas the Kaplan-Meier curve was used for survival analysis.
Results
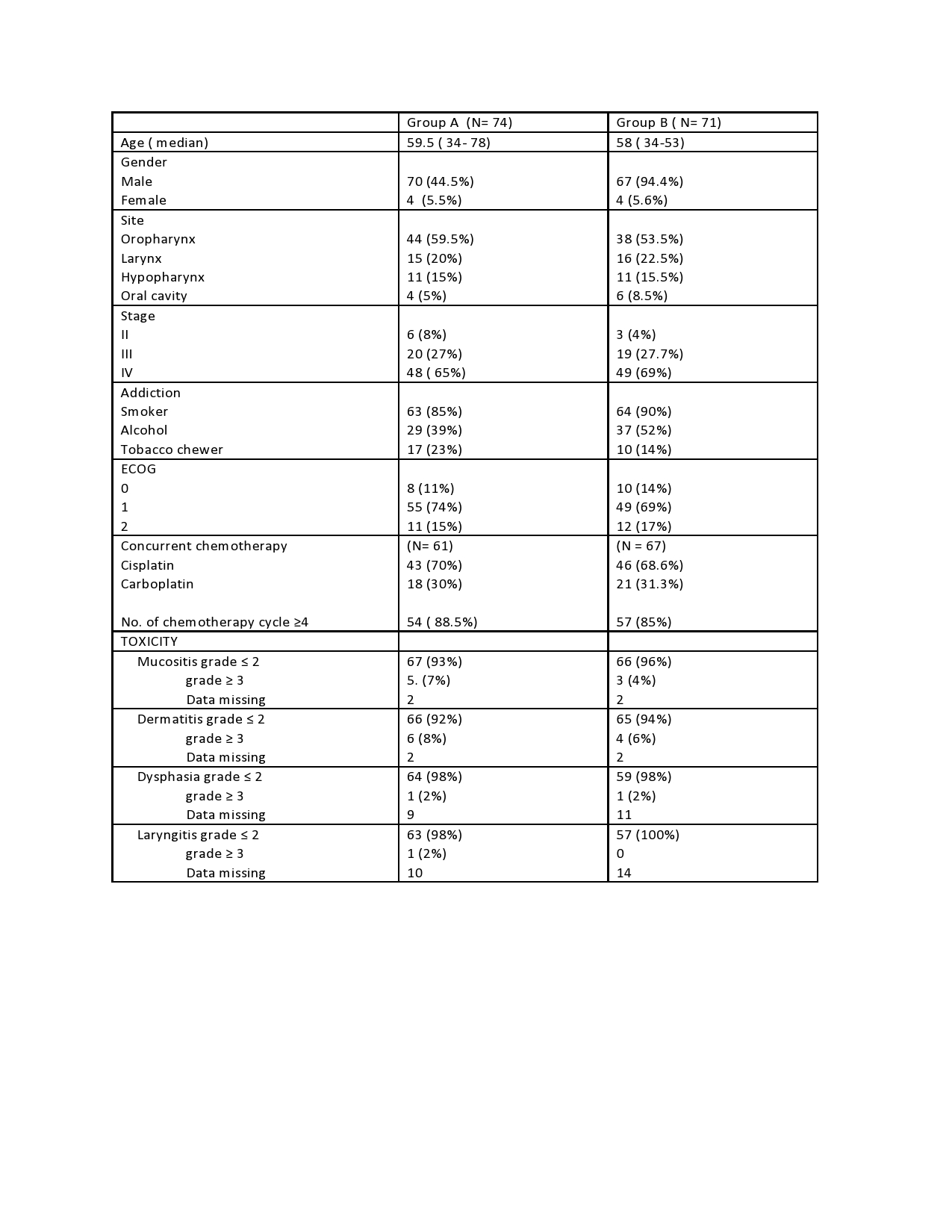
A total of 145 patients were assessed for final analysis. Group A consists of 74 patients, while Group B consists of 71 patients. The following table shows the clinico-demographic profile of the patients.The median duration of treatment completion in groups A and B was 46 (40–117) and 49 (44–102) days, respectively. Patients requiring hospital admission due to treatment toxicity and nutritional support were 20 (27%) in group A and 9 (12%) in group B. At 3 and 6 months of follow-up, the complete response (CR) observed in both the groups was 68.2% vs 70.1% and 66.1% vs 66.6%, respectively (p = 0.15).
Conclusion
The toxicity profile and local control in both these fractionation schedules are almost similar, with a trend towards better overall survival in Arm-A. Although as per our study, 66Gy in 30# seems to be a better alternative in high volume centres, a prospective randomised trial comparing both this fractionation and the other is to be conducted in future to establish this result with a higher level of evidence.