MCO-based training of RapidPlan for lung cancer improves sparing of heart and oesophagus
Liv Bolstad Hysing,
Norway
PO-1623
Abstract
MCO-based training of RapidPlan for lung cancer improves sparing of heart and oesophagus
Authors: Marte Hordnes1,2, Kristine Fjellanger1,2, Inger Marie Sandvik2, Ben J. M. Heijmen3, Sebastiaan Breedveld3, Linda Rossi3, Turid Husevåg Sulen2, Helge Egil Seime Pettersen2, Liv Bolstad Hysing1,2
1University of Bergen, Department of Physics and Technology, Bergen, Norway; 2Haukeland University Hospital, Department of Oncology and Medical Physics, Bergen, Norway; 3Erasmus University Medical Center, Department of Radiotherapy, Rotterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Manual IMRT treatment planning of non-small cell lung cancer (NSCLC) can be complex and plan quality may depend on the experience of the dosimetrist and available time. Automated multi-criterial optimization (MCO) has shown potential to enhance radiotherapy, also for NSCLC. In the current study, we have investigated if MCO could be used to improve training of our clinically available RapidPlan-system and thereby indirectly enhance plan quality in a clinic without routine access to automated MCO.
Material and Methods
Forty patients with inoperable NSCLC (stage IB-IVA) receiving curative 6-field IMRT with prescribed dose of 60-70 Gy in 2 Gy fractions, were prospectively included in this study. The patients were split into a training (n=30) and validation group (n=10). All patients had available the manually planned clinical IMRT-plan as well as an automated MCO treatment plan with improved sparing of the heart and oesophagus. For the training group, these plans were used as input for RapidPlan-models RP_CLIN and RP_MCO, respectively. We initially created and validated the RP_CLIN model compared to the clinical IMRT-plan. Thereafter we compared RP_CLIN and RP_MCO using relevant dose/volume metrics (PTVV95%, Lungs Dmean, V5Gy and V20Gy, Heart Dmean, V5Gy and V30Gy, Oesophagus Dmean, V20Gy and V60Gy and Spinal Canal Dmax). Lastly, the responsible oncologist evaluated for the validation patients the clinical, RP_CLIN and RP_MCO dose distributions while blinded for technique.
Results
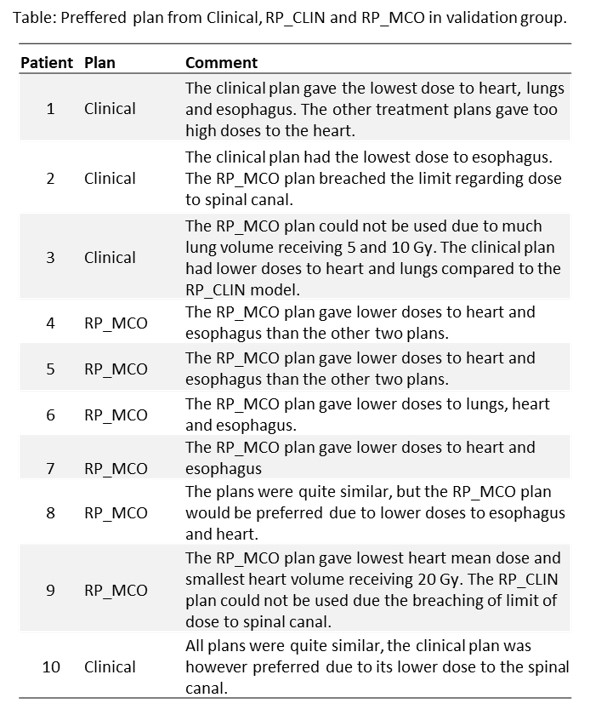
Satisfactory training (average R2 of 0.79 and average X2 of 1.01) and closed-loop validation-results were obtained with RP_CLIN. In open-loop validation, no significant difference (p>0.05) between the clinical IMRT-plan and RP_CLIN were found for PTV or OARs except for the max dose to the spinal canal that was higher in RP_CLIN (median 49.2 Gy vs 45.4 Gy, p=0.022 Wilcoxon). Compared to RP_CLIN, RP_MCO significantly improved heart V30Gy (median 6.7% vs 7.2%, p=0.005), oesophagus Dmean (median 19.6 Gy vs 20.0 Gy, p=0.022) and V60Gy (4.8% vs. 6.4%, p=0.028). Both Rapidplan-models were thus feasible, but the spinal canal max dose criteria could be tuned. The oncologist preferred RP_MCO in 6 out of 10 patients and the clinical IMRT-plan in four patients. The RP_CLIN plan was not preferred in any of the patients (Figure). A lower heart and oesophagus dose were the main reasons for choosing RP_MCO while there were various reasons for choosing the clinical IMRT-plan (Table).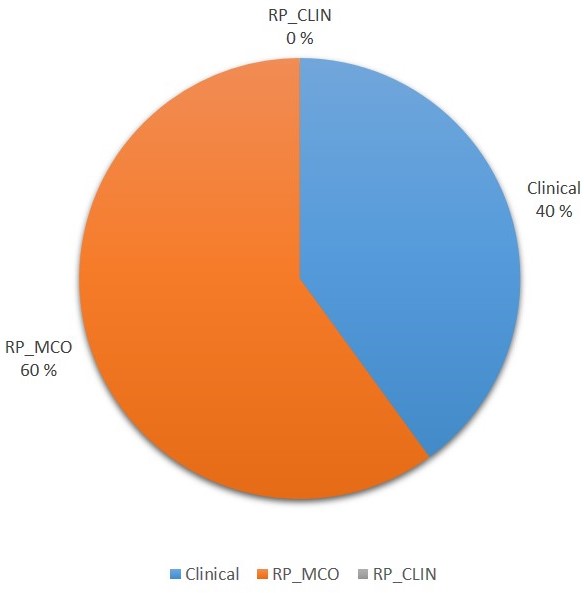
Conclusion
RP_MCO improved sparing of the heart and oesophagus compared to RP_CLIN. In the choice between RP_MCO, RP_CLIN and Clinical, RP_MCO was selected for 60% of patients and RP_CLIN was never selected.