Lung re-irradiation with SBRT: outcomes and predictive factors of response in the recurrent setting
PD-0963
Abstract
Lung re-irradiation with SBRT: outcomes and predictive factors of response in the recurrent setting
Authors: Ilaria Angelicone1, Margherita Rotondi1, Riccardo Carlo Sigillo1, Paolo Bonome2, Donatella Caivano3, Maurizio Valeriani1, Mattia Falchetto Osti1
1Università degli Studi di Roma "La Sapienza", A.O.U. Sant'Andrea M-P, Radiation Oncology, Rome, Italy; 2Gemelli Molise Hospital Department of Laboratories and Services, Radiation Oncology, Campobasso, Italy; 3Santa Maria Goretti Hospital, Radiation Oncology, Latina, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Patients (pts) with primary or secondary lung lesions previously irradiated can experience a locoregional failure or the appearance of new lung lesions, thus requiring a thoracic re-irradiation. In this setting Stereotactic Body Radiation Therapy (SBRT) represents an optimal treatment modality due to its high local control rate with acceptable risk of complications. Aim of this monoinstitutional retrospective study is to evaluate outcomes and predictive factors of response of SBRT in the recurrent setting.
Material and Methods
From April 2011 to October 2021, 42 pts (29 males, 13 females) received re-irradiation of lung lesions by SBRT. Median time between the two treatment was 24.6 months (range: 3-92). Median age was 73 years (range: 47-88). All pts had an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0–2. Of the 56 total lesions, primary cancer was lung in 57%, colon-rectal in 16%, not-typable in 11%, breast in 9%, endometrial and oropharyngeal in 3.5% respectively. Thirty-four lesions were treated in the same lobe, 12 in the ipsilateral lobe, 10 in the contralateral lung. Fifty-four lesions were peripherally located and 2 had a central location. Medium volume of clinical target volume (CTV) was 32.75 cc (range: 0.89-260.77). Medium BED10 of re-irradiation was 97.8 Gy (range: 37.5-151.2) and medium EQD210 was 82.18 Gy (range: 31.25-126). Thirteen lesions were re-irradiated with a single fraction, 43 with multiple fractions (range: 3-10). The most represented schedules in all subsequent courses of SBRT were 30 Gy in 1 fraction, 45 Gy in 3 fractions and 54 Gy in 3 fractions.
Results
After a median follow-up of 24.8 months (range: 3.2-141.7), Local Control (LC) was 53.2% at 1-year, 50.6% at 2-years and 35.5% at 3-years. Progression Free Survival (PFS) was 37.8% at 1- year, 28.1% at 2-years and 10.5% at 3-years. Disease Specific Survival (DSS) was 76.6 % at 1-year, 47.4% at 2-years and 36.9% at 3-years. Overall Survival (OS) was 78.3% at 1-year, 49.5% at 2-years and 40.1% at 3-years. On univariate analysis, CTV volume ≥ 33cc was statistically significantly related to LC (p=0.0157) and PFS (p=0.0106). Total number of treatments on lungs had a statistically significant correlation to PFS (p=0.0188), DSS (p=0.0007) and OS (p=0.0017). Number of re-irradiations was significantly related to PFS (p=0.0300) and DSS (p=0.0011).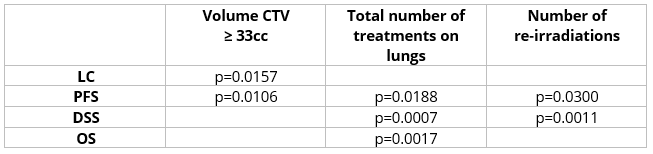
Conclusion
Our experience showed favorable long-term outcomes in pts retreated on lung with SBRT. Data on role of SBRT in recurrent setting are limited and further studies are necessary to confirm feasibility and safety of this approach.