GEC-ESTRO Best Junior Presentation: EviGUIDE - A tool for evidence-based decision making in image-guided adaptive brachytherapy
OC-0134
Abstract
EviGUIDE - A tool for evidence-based decision making in image-guided adaptive brachytherapy
Authors: Stefan Ecker1, Christian Kirisits1, Maximilian Schmid1, Johannes Knoth1, Gerd Heilemann1, Astrid Agatha Catharina De Leeuw2, Alina Emiliana Sturdza1, Kathrin Kirchheiner1, Sofia Spampinato3, Kari Tanderup3, Richard Pötter1, Nicole Eder-Nesvacil1
1Medical University of Vienna, Department of Radiation Oncology, Comprehensive Cancer Center, Vienna, Austria; 2University Medical Centre Utrecht, Department of Radiation Oncology, Utrecht, The Netherlands; 3Aarhus University Hospital, Department of Oncology, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
The software tool EviGUIDE should enhance the traditional treatment planning workflow in radiation oncology (RO). It combines dosimetric information from the treatment planning system (TPS), patient and treatment characteristics and established tumor control probability (TCP), and normal tissue complication probability (NTCP) models, to extend the assessment of treatment plan quality beyond adherence to rigid dose objectives.
Material and Methods
The concept is demonstrated for the treatment of cervical cancer using combined external beam radiotherapy and magnetic resonance image-guided adaptive brachytherapy (MR-IGABT). The tool was developed using R and Python. A software link to a TPS enables usage alongside routine treatment planning. It provides users with outputs for dose documentation based on equieffective dose in 2 Gy per fraction (EQD2), advanced visualizations, and statistical summaries of a treatment plan. Using uniform dose scaling for the entire or fractionated BT dose distribution, users are able to dynamically create alternative versions of the treatment plan and compare them via EQD2 parameters and in the TCP-NTCP space.
In total, six Cox Proportional Hazards models based on outcome data from the multi-national EMBRACE-I study have been integrated. One TCP model for local tumor control, and five NTCP models for CTCAE Grade ≥ 2 morbidity endpoints. To quantify the optimization potential among patients treated with state-of-the-art MR-IGABT, a mono-institutional retrospective cohort of 45 patients was analyzed. Plans were optimized by scaling the dose distribution until the maximum attainable TCP within existing dose limits was achieved.
Results
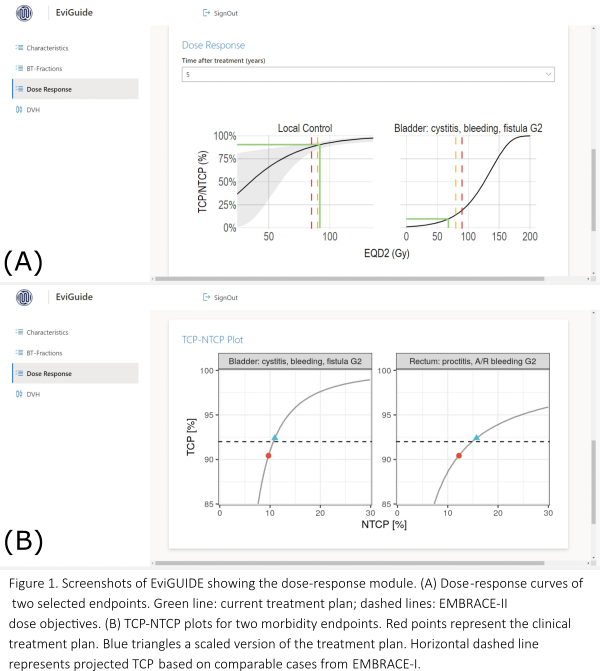
A prototype was developed that can be run locally or on a webserver. It allows automatic import of dose-volume histograms (DVH) from a commercial TPS and the selection of patient specific clinical and treatment characteristics. EviGUIDE outputs include standard EQD2 dose documentation, attainable TCP/NTCP (Fig. 1) and boxplots of DVH parameters based on patient cohorts according to the specific treatment situation.
Optimization of treatment plans revealed that for a sub-cohort of patients with increased risk factors (20%, 9/45), an average gain in TCP of 2% would have been possible, while increasing the risk for Grade ≥ 2 side-effects by up to 2% (Tab. 1). Overall, the retrospective analysis showed that individual cases would have greatly benefited from the quantitative and visual feedback of EviGUIDE.
Conclusion
The decision support software EviGUIDE provides guidance on individualized dose prescription and allows users clear communication of expected treatment outcome based on model predictions, and insights about trade-offs between local tumor control and organ at risk sparing. Utility and potential dose variation approaches should be tested prospectively in a clinical protocol. It can aid the dissemination of evidence-based knowledge about optimal treatment, and serve as a blueprint for other sites in RO.