Dosimetric risk factors for vaginal and sexual toxicity in locally advanced cervix cancer
OC-0133
Abstract
Dosimetric risk factors for vaginal and sexual toxicity in locally advanced cervix cancer
Authors: Alexandra Rink1,2,3, Jennifer Hanuschak4, Leigh Conroy1,2, Kathy Han4,2, Mike Milosevic4,2, Jelena Lukovic4,2, Sarah Ferguson5, Ailya Salman5, Anna Santiago6, Jessica L Conway7,2, Jennifer Croke4,2
1University Health Network, Medical Physics, Toronto, Canada; 2University of Toronto, Radiation Oncology, Toronto, Canada; 3University of Toronto, Medical Biophysics, Toronto, Canada; 4University Health Network, Radiation Medicine Program, Toronto, Canada; 5University of Toronto, Gynecologic Oncology, Toronto, Canada; 6University Health Network, Biostatistics, Toronto, Canada; 7Royal Victoria Regional Health Centre, Radiation Oncology, Barrie, Canada
Show Affiliations
Hide Affiliations
Purpose or Objective
HDR brachytherapy (BT) plays a critical role in the treatment of locally advanced cervical cancer. Our objective was to identify relationships between physician reported vaginal toxicity (VT) and patient reported sexual health outcomes (PROs) with dosimetric markers of HDR-BT in locally advanced cervix cancer.
Material and Methods
This was a single-centre prospective cross-sectional study of Stage IB-IVA cervical cancer patients treated with definitive CRT and MR-guided BT who were disease-free for >3 months. Consenting patients completed validated PROs: Female Sexual Distress Scale-Revised (FSDS-R), Female Sexual Function Index (FSFI), and Menopause Rating Scale (MRS), as well as a socio-demographics questionnaire. Physicians prospectively scored VT using the CTCAE v4.0. Dosimetric markers are: equivalent dose in 2 Gy fractions (EQD2) for Vaginal D2cm and ICRU recto-vaginal (RV) point, maximum fractional Vaginal D2cc (MaxVagD2cc), maximum fractional point dose, MaxVagPoint, (among ICRU-RV and vaginal lateral points 5 mm from applicator), EQD2 for MaxVagPoint, maximum fractional vaginal total reference air kerma (TRAK), (MaxVagTRAK), and total vaginal TRAK (TotalVagTRAK). To explore associations with dosimetry, unadjusted univariate linear regression was performed for each variable as a function of PROs, physician assessed VT and clinical covariates.
Results
Between August 2018 and April 2022, 78 patients were enrolled and 74 completed PROs. Median age at diagnosis was 49.5 (range: 25-81), 51% were FIGO cT2b, and 61% had vaginal involvement at diagnosis. 76 patients received EBRT of 45Gy in 25 with/without simultaneous nodal boost or post-brachy nodal boost. 77 patients received 28Gy/4fx or 24Gy/3 fx HDR-BT. Median time from treatment was 19.8 months (3.3-57.1). Median HR-CTV D90 was 92.1Gy (81-106.4), ICRU-RV point was 61.8Gy (49.8-118.5) and vaginal D2cc was 76.8 Gy (54.7-133). Correlations between PROs, physician assessed VT and clinical data are summarized in Table 1. Dose to ICRU-RV and vaginal points were independently correlated with vaginal involvement at BT.
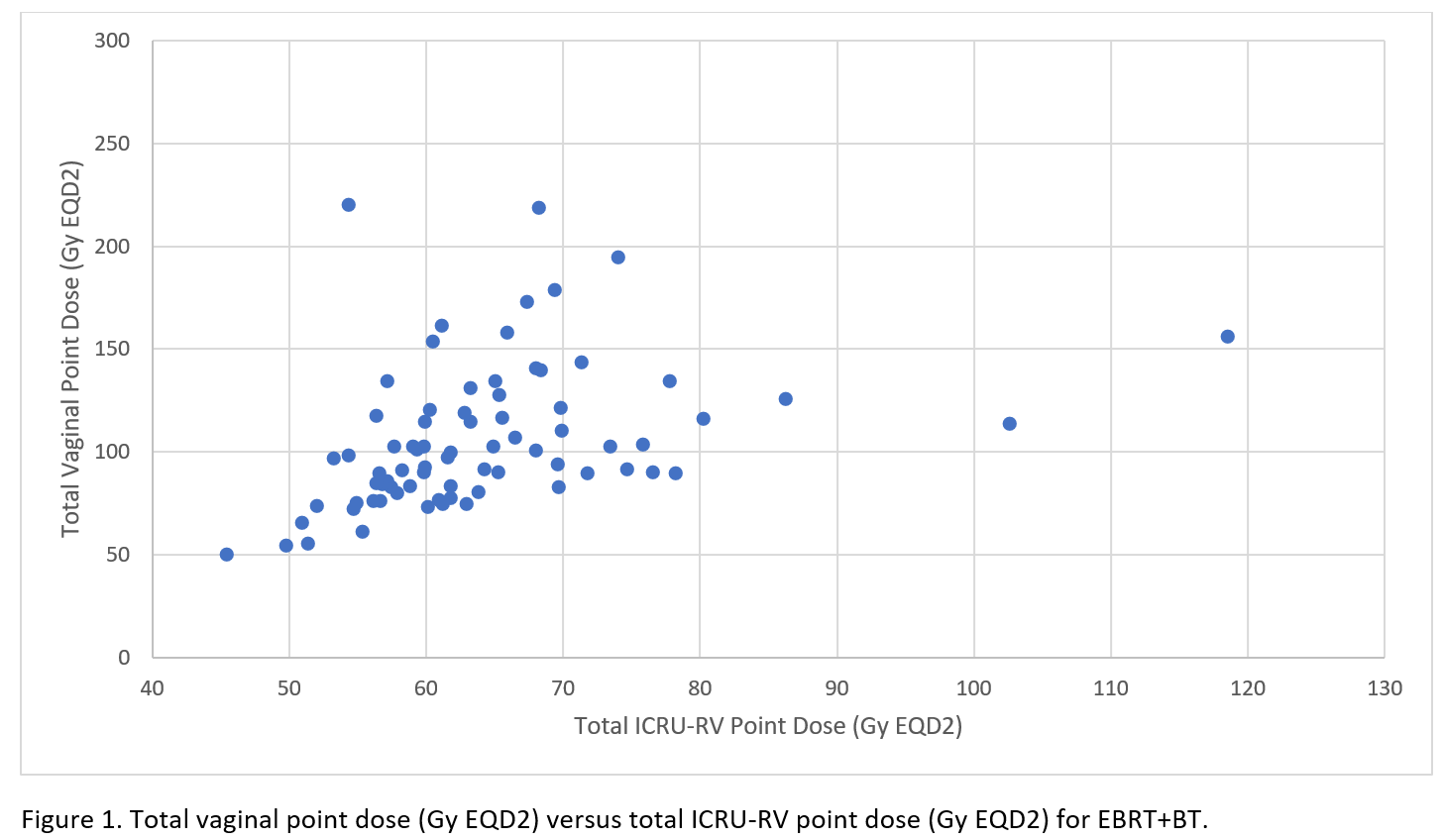
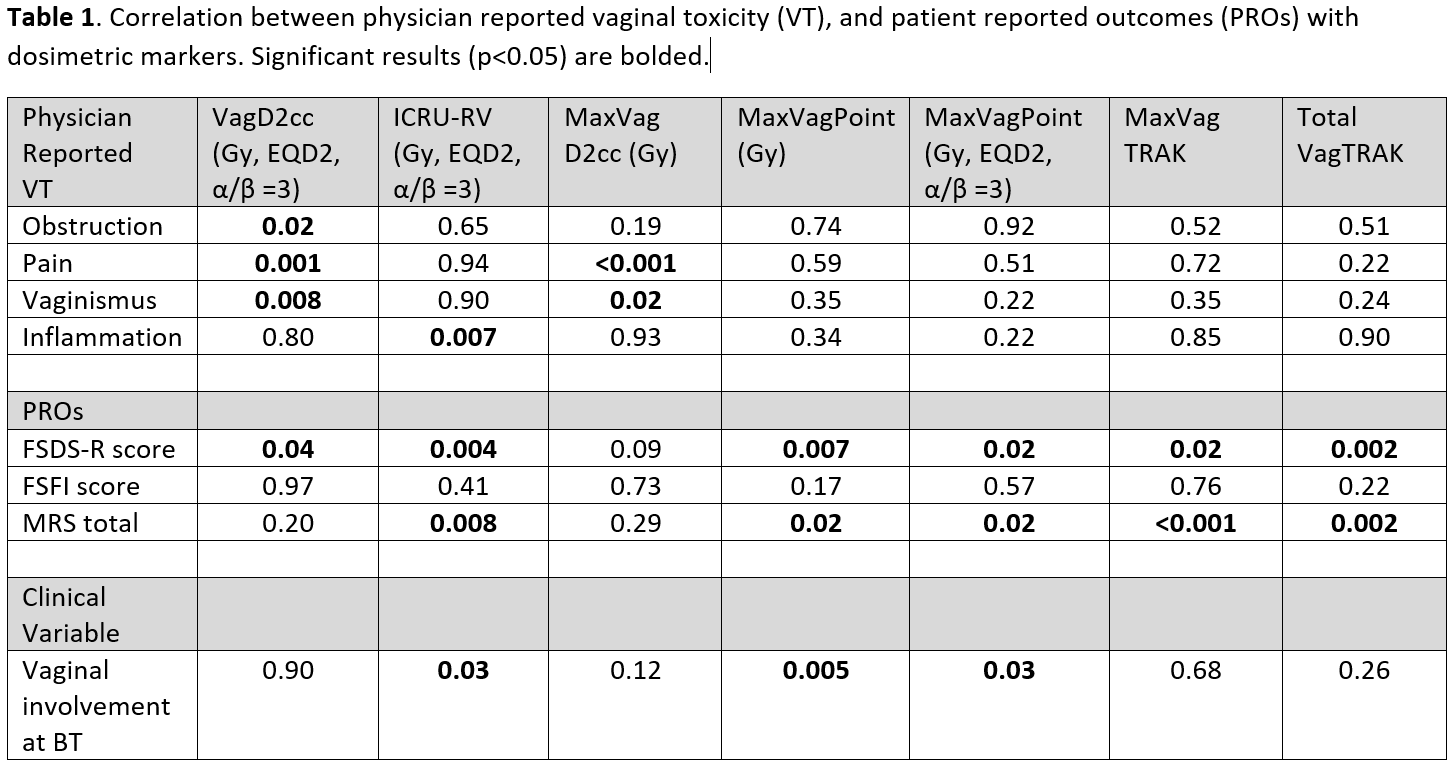 There is a significant positive association between total ICRU-RV point dose and FSDS-R, MRS, and physician assessed VT. Those with ICRU-RV >65 Gy had a significantly higher FSDS-R and MRS scores compared to those with ICRU-RV <65 Gy (p=0.02). Furthermore, there is a significant positive association between MaxVagPoint and MaxVagPoint EQD2 and FSDS-R, and MRS. MaxVagTRAK and TotalVagTRAK have a significant positive association with FSDS-R score and MRS. MaxVagPoint doses typically greatly exceed values of ICRU-RV (Figure 1).
There is a significant positive association between total ICRU-RV point dose and FSDS-R, MRS, and physician assessed VT. Those with ICRU-RV >65 Gy had a significantly higher FSDS-R and MRS scores compared to those with ICRU-RV <65 Gy (p=0.02). Furthermore, there is a significant positive association between MaxVagPoint and MaxVagPoint EQD2 and FSDS-R, and MRS. MaxVagTRAK and TotalVagTRAK have a significant positive association with FSDS-R score and MRS. MaxVagPoint doses typically greatly exceed values of ICRU-RV (Figure 1).
Conclusion
This analysis indicates that there is a significant relationship between dosimetric markers and physician-reported VT and patient-reported sexual health outcomes. Opportunities exist for accurate identification of an appropriate vaginal D2cc, point-dose and TRAK constraints, de-escalating vaginal dose and reducing sexual morbidity.