Which is the optimal lymph node management in node positive cervical cancer?
Alexandru-Teodor Zaharie,
Austria
OC-0603
Abstract
Which is the optimal lymph node management in node positive cervical cancer?
Authors: Alexandru-Teodor Zaharie1, Alina Sturdza1, Johannes Knoth1, Christoph Grimm2, Stephan Polterauer2, Christian Kirisits1, Richard Pötter1, Joachim Widder1, Maximilian Schmid1
1Medical University of Vienna, Radiation Oncology, Vienna, Austria; 2Medical University of Vienna, Gynaecology, Vienna, Austria
Show Affiliations
Hide Affiliations
Purpose or Objective
To analyze the impact of different lymph node (LN) management strategies on regional lymph node control (RNC) in patients with LN positive locally advanced cervical cancer (LACC) undergoing definitive chemoradiation (CRT) and image guided adaptive brachytherapy (IGABT).
Material and Methods
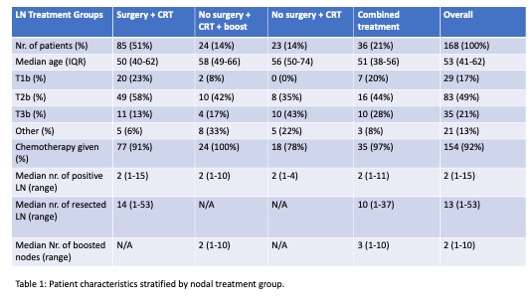
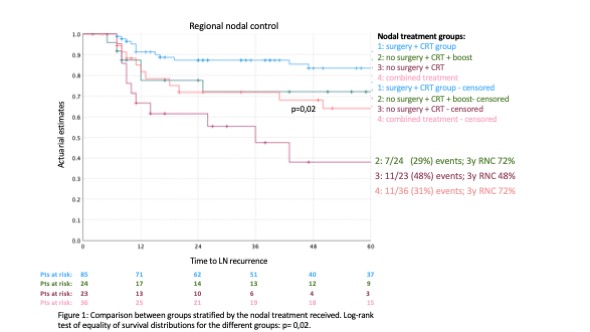
All patients with pelvic and/or paraaortic nodal disease at diagnosis (FIGO stage IIIC1-2) treated at the Medical University of Vienna within the retrospective retroEMBRACE study and the prospective EMBRACE I and II studies were considered for analysis. Patients were stratified according to the respective LN management: (1) surgical staging (either as LN sampling and/or debulking = limited surgical staging; or as an extended lymphadenectomy = extended surgical staging) with complete resection of all suspicious LN disease followed by 45-50.4Gy CRT (surgery + CRT group); (2) 45-50.4Gy CRT + LN boost up to 60Gy without surgical staging (no surgery + CRT + boost); (3) 45-50.4Gy CRT without LN boost or surgical staging (no surgery + CRT); (4) incomplete surgical staging or remaining suspicious LN followed by 45-50.4Gy CRT with or without LN boost (combined treatment group). RNC was defined as the absence of pelvic and paraaortic LN recurrence at 3 years and was calculated using the Kaplan-Meier method by comparing LN management groups with log-rank tests.
Results
With a median follow-up of 40 months (IQR 12-88) 168 patients were available. Patient characteristics for the overall cohort and broken down by LN management group are shown in table 1. Overall, 3-year actuarial RNC was 77%. Three-year RNC per LN management group are displayed in figure 1). Surgical management followed by CRT showed a significantly improved in RNC compared to the CRT-only group (87% vs. 49%, p< 0,01), while an additional LN boost in suspicious LN at CRT seemed to also improve 3-year RNC (72% vs. 48%), albeit not reaching statistical significance (p=0,14). The type of surgical management had no significant impact on RNC (p=0,283).
Conclusion
In this single center cohort analysis surgical resection and/or RT boost of macroscopic nodal disease in LACC suggest superior RNC in patients with LACC. These findings underline the need for an additional LN therapy to standard 45-50.4Gy CRT.