Prostate Virtual HDR Brachytherapy Boost: 5-year Prospective Multicentre Clinical Trial Results
OC-0926
Abstract
Prostate Virtual HDR Brachytherapy Boost: 5-year Prospective Multicentre Clinical Trial Results
Authors: Jarad Martin1, Mark Sidhom2, David Pryor3, Joseph Bucci4, Eric Wegener5, Kenway Yeoh5, Matthew Richardson5, Peter Greer5, Sarah Gallagher5, Lee Wilton5, Laurel Schmidt4, Sarah Keats6, Sankar Arumugam6, Simon Brown3, Alan Glyde3
1Calvary Mater Newcastle, Radiation Oncology, Newcastle, Australia; 2Liverpool Hospital, Department of Radiation Oncology, Liverpool, Australia; 3Princess Alexandra Hospital, Department of Radiation Oncology, Brisbane, Australia; 4St George Hospital, Department of Radiation Oncology, Sydney, Australia; 5Calvary Mater Newcastle, Department of Radiation Oncology, Newcastle, Australia; 6Liverpool Hospital, Department of Radiation Oncology, Sydney, Australia
Show Affiliations
Hide Affiliations
Purpose or Objective
Despite superior efficacy from High Dose Brachytherapy Boost (HDRB), use of this approach is declining for many reasons including diminishing subspecialist expertise, high rates of significant genitourinary (GU) toxicity and intensive resourcing requirements. Similar dosimetry can be achieved using SBRT, or ‘Virtual HDRB’. Here we report on 5-year outcomes of Virtual HDRB from a prospective, phase 2, multicentre study (PROMETHEUS: ACTRN12615000223538).
Material and Methods
Patients with intermediate or selected high risk prostate cancer were treated with linac-based SBRT, 19–21 Gy in two fractions delivered 1 week apart, followed by conventionally fractionated IMRT (46 Gy in 23 or 36 Gy in 12 fractions). MRI fusion for RT planning, rectal displacement, and intrafraction image guidance were mandated. The primary endpoint was biochemical-clinical control via the Phoenix definition. Toxicity was graded using CTCAE v4 and quality of life (QoL) data analysed using the EPIC-26 questionnaire.
Results
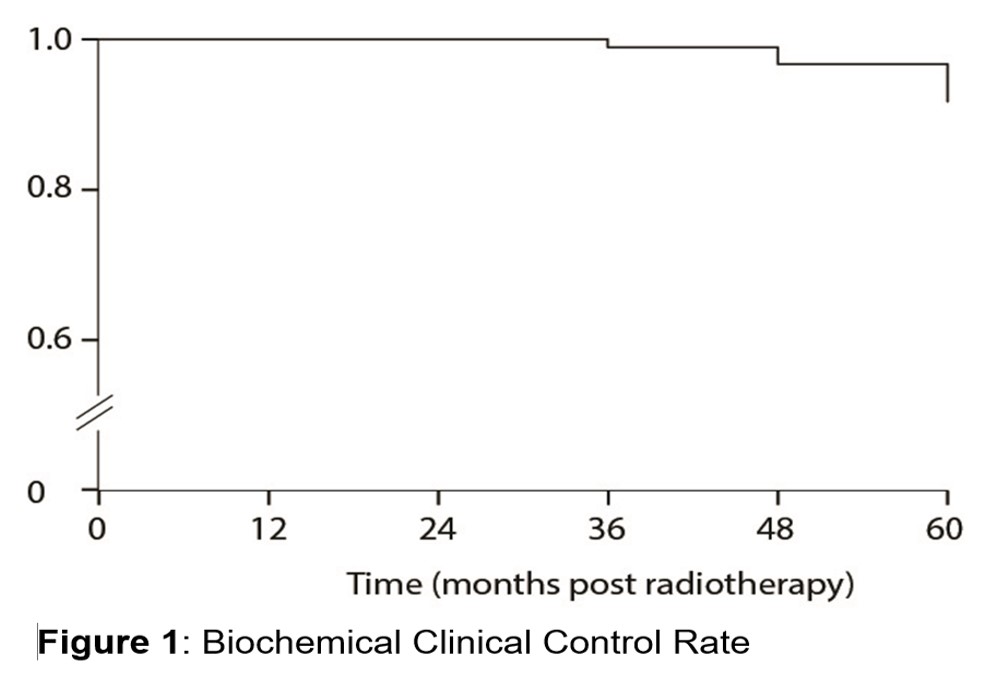
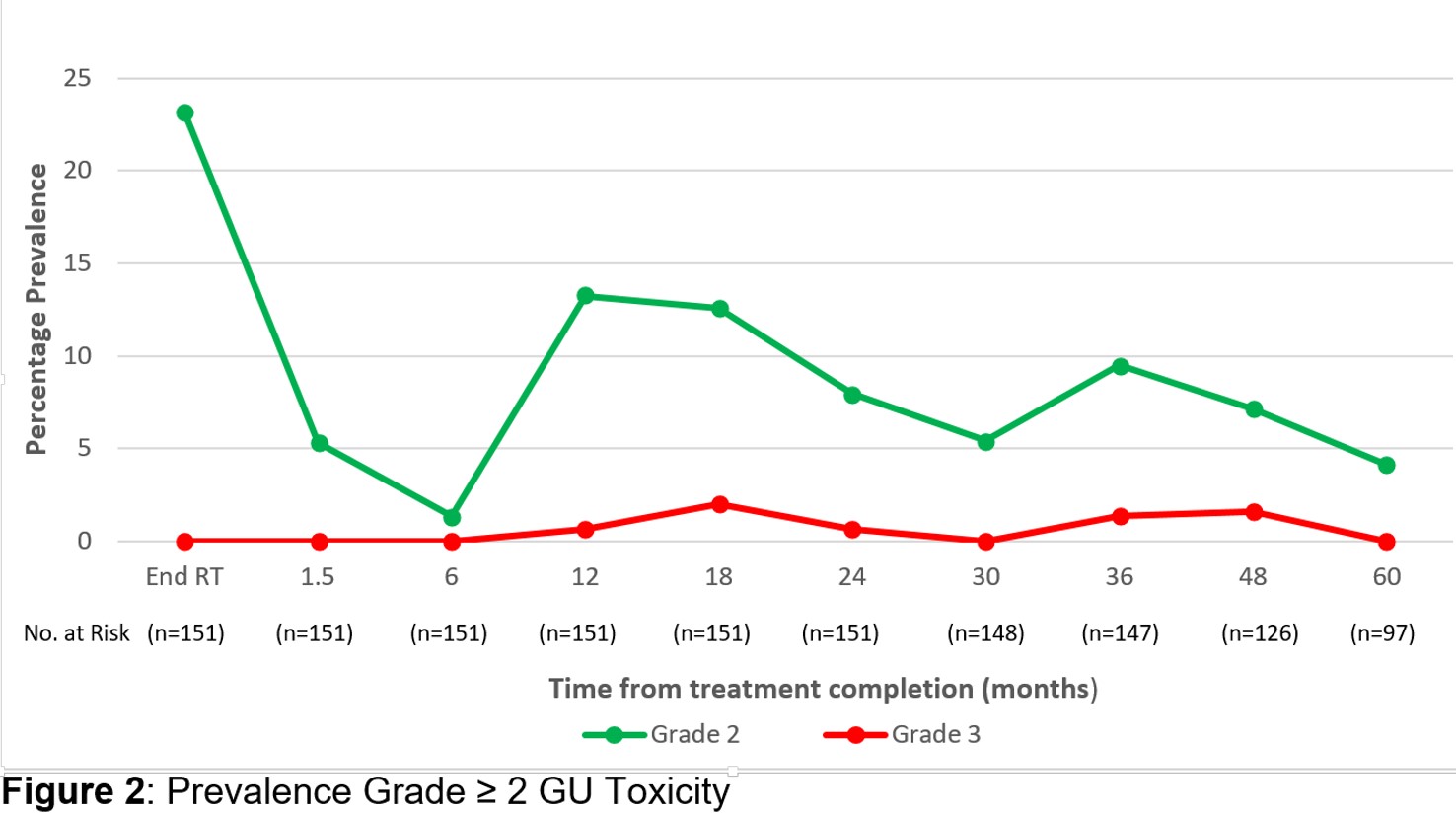
From March 2014 to December 2018, 151 patients (74% intermediate, 26% high-risk) with a median age of 69 were treated across five centres. Short course (≤6 months) ADT was used in 36% and long course in 19%. Elective pelvic nodal treatment was given in 10% of patients. Median follow-up was 60 months. The 5-year biochemical clinical control rate was 93.4% [95% CI 88-96%, fig 1]. Local control was 99.3% with one local failure. Acute grade 2 gastrointestinal (GI) and GU toxicity occurred in 6.6% and 23.2% with no acute grade 3 toxicity. At 6, 12, 24, and 60 months post-treatment the prevalence of late grade ≥2 GI toxicity was 1.3, 3.3, 1.3 and 1.0%, respectively, and the prevalence of late grade ≥2 GU toxicity was 1.3, 13.2, 7.9 and 4.1%, respectively (fig 2). Five patients experienced grade 3 late toxicities which subsequently resolved to grade 2 or less. No man experienced a urethral stricture. For the 68 men not receiving ADT, the median PSA value pre-treatment was 7.33 µg/L (1.1–20µg/L) and at 12, 24, 36, 48 and 60 months post-treatment was 0.86, 0.375, 0.21, 0.13, and 0.075 µg/L. The irritative/obstructive urinary QoL domain showed continued improvement after treatment compared to baseline (+4 points on a 100 point normalised scale; p = 0.017) while both urinary incontinence QoL and sexual QoL declined (-7 and -9 points respectively; both p <0.01). There were no significant changes in the bowel domain over 60 months.
Conclusion
Delivery of a gantry-based SBRT boost followed by conventional fractionated IMRT is feasible in a multicentre setting and resulted in excellent 5 year biochemical clinical control. Rates of early and late GU toxicities were acceptable, there were minimal GI toxicities, and changes in QoL domains were consistent with prostate cytoreduction and aging. This promising regimen is being evaluated in a randomised trial compared with 40Gy in 5 fractions of SBRT monotherapy (TROG 18.01 NINJA ACTRN12618001806257).