A complete bilateral model of lymphatic progression in HNSCC trained with multicentric patient data
Roman Ludwig,
Switzerland
OC-0087
Abstract
A complete bilateral model of lymphatic progression in HNSCC trained with multicentric patient data
Authors: Roman Ludwig1, Jean-Marc Hoffmann1, Bertrand Pouymayou1, Luca Franceschetti2, Laurence Bauwens3, Vincent Grégoire3, Panagiotis Balermpas1, Jan Unkelbach1
1University Hospital Zurich, Radiation Oncology, Zurich, Switzerland; 2Univerity of Zurich, Physics, Zurich, Switzerland; 3Centre Léon Bérard, Radiation Oncology, Lyon, France
Show Affiliations
Hide Affiliations
Purpose or Objective
The elective clinical target volume (CTV-N) in oropharyngeal squamous cell carcinoma (OPSCC) is currently defined using guidelines [1] based on the prevalence of metastasis by lymph node level (LNL). These guidelines recommend extensive irradiation of both sides of the neck for most patients, but do not consider how the patient-specific risk to harbor occult disease changes based on the individual's clinical diagnosis. We developed a statistical model to quantify the risk of occult disease in any LNL, given an individual patient’s T-category, tumor lateralization, and clinical extent of nodal metastasis.
Material and Methods
We extended a previously developed hidden Markov model (HMM) of lymphatic progression in OPSCC [2] to include all relevant LNLs (I, II, III, IV, V, and VII) for both the ipsi- and the contralateral side. A tumor’s extension over the mid-sagittal plane is included as a risk factor for contralateral involvement. The state of each LNL (involved/healthy) is represented by binary random variables; lymphatic drainage is represented by directed arcs between the LNLs and are parametrized with spread probabilities. The model parameters are learned from two large OPSCC datasets from the USZ (CH) and the CLB (FR) (550 patients, see lyprox.org). Bayesian model comparison is used to determine the graph of the model that best describes the data.
Results
Fig. 1 compares the observed prevalence of involvement in the data (solid lines) and the model's prediction (shaded histograms) for different combinations of LNLs, T-category, and midline extension. To represent uncertainty in both the data and the model, the data is represented via Beta distribution over the observed prevalence while the model is represented via histograms obtained by sampling from the joint probability distribution over the model parameters. These comparisons show the HMM’s capability to fit to the dataset including the dependence of LNL involvement on T-category and midline extension.
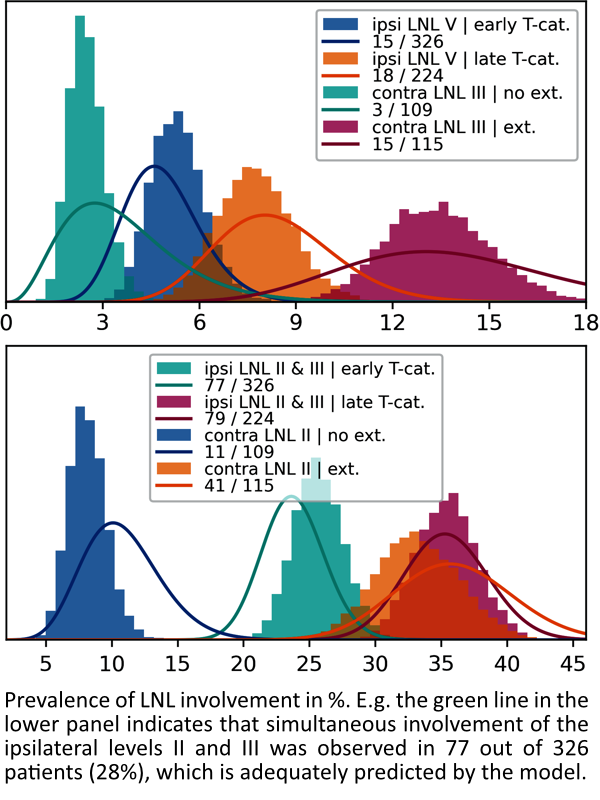
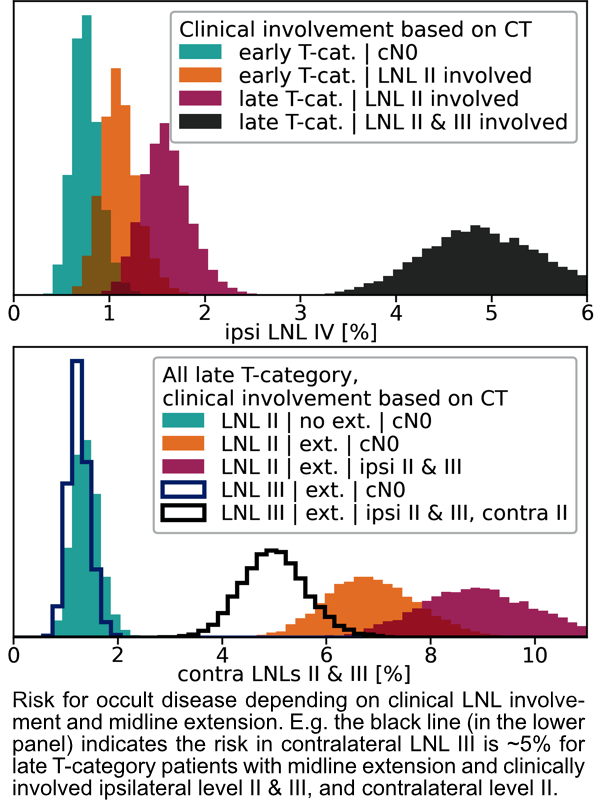
Fig. 2 shows the model's predicted risks of occult metastases assuming imaging-based diagnosis of lymph node metastases with a sensitivity of 81% and a specificity of 76% [3]. The top panel in fig. 2 shows that the predicted risk for occult metastases in ipsilateral LNL IV only exceeds ~5% if the up-stream LNLs II and III harbor metastases. Similarly, the bottom panel shows that the risk in contra-lateral level III only exceeds ~5% if contralateral level II harbors metastases. The risk in contralateral level II exceeds ~5% except for lateralized tumors.
Conclusion
The HMM model may inform future clinical trials on volume-deescalated radiotherapy for OPSCC. Assuming a 5% threshold, it indicates that irradiation of ipsilateral LNL IV may not be required when nodal disease is limited to level II. In addition, contralateral irradiation may be limited to level II for patients without contralateral metastases.
References:
- Biau (2019) Rad. & Onc. 134 1-9
- Ludwig (2021) Sci. Rep. 11 12261
- de Bondt (2007) Eur. J. Radiol. 64 266-272