Are MRI scans needed for precise image-based data mining in paediatric brain tumour cohorts?
Abigail Bryce-Atkinson,
United Kingdom
OC-0776
Abstract
Are MRI scans needed for precise image-based data mining in paediatric brain tumour cohorts?
Authors: Abigail Bryce-Atkinson1, Eliana Vasquez Osorio1, Andrew Green2, Austin M Faught3, Martin G McCabe1, Thomas E Merchant3, Marcel van Herk1, Marianne C Aznar1, Lydia J Wilson3
1The University of Manchester, Division of Cancer Sciences, Faculty of Biology, Medicine and Health, Manchester, United Kingdom; 2European Bioinformatics Institute, European Molecular Biology Laboratory, Hinxton, United Kingdom; 3St Jude Children's Research Hospital, Department of Radiation Oncology, Memphis, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Image-based data mining (IBDM) is a voxel-wise technique for identifying spatial dose-response associations in radiotherapy. IBDM spatially normalises 3D imaging and dose distributions to a reference anatomy prior to computing ‘per-voxel’ correlations of dose and clinical outcomes. Applying IBDM in paediatric cancer cohorts often requires multi-institutional collaborations to achieve appropriate cohort s for analysing long-term retrospective data. A particular challenge for IBDM brain-tumour research is that although MRI is indicated due to superior anatomical definition, it may not be as readily available as CT in historical cohorts. This work compares results from MRI- and CT-based IBDM pipelines to evaluate the impact of using MRI for IBDM paediatric studies in the brain.
Material and Methods
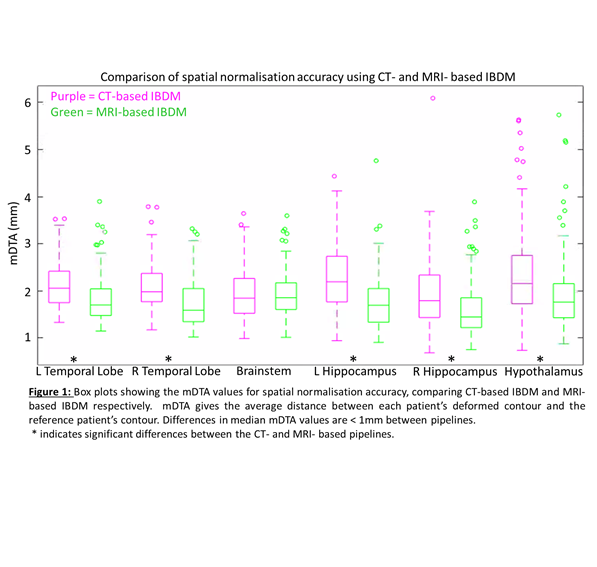
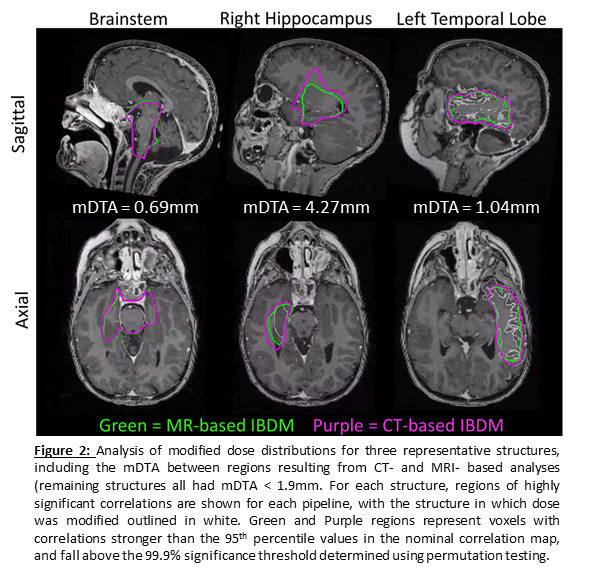
We used CT, MRI, radiotherapy dose and contours from 128 children who received curative craniospinal irradiation for Medulloblastoma. Spatial normalisation was performed by non-rigidly registering each patient’s scan to the patient with the median brain volume. We quantified spatial normalisation accuracy by comparing each patient’s mapped structure contours to the corresponding reference contours via mean distance to agreement (mDTA). To standardize the dose comparison, we created modified dose distributions by replacing the dose in 5 structures (Figure 1) with the mean dose in that structure and simulated outcome labels, assigning “effect” labels to patients whose mean structure dose exceeded the median dose of the cohort. Per-voxel dose comparisons used permutation testing (1000 permutations) to identify voxel clusters in which the dose was significantly associated with the simulated outcome labels. Identified significant clusters were compared between the CT- and MRI-based pipelines via mDTA. In this test, the “ideal” IBDM result would be significant clusters of voxels that match the structure containing the dose modification.
Results
We found significant differences (Wilcoxon signed-rank test) in spatial normalisation between CT- and MRI- based pipelines (p<0.001, Figure 1), however the magnitude of these differences was small (<1 mm). Both IBDM pipelines identified clusters containing the modified dose region ( > 99.9% significance, i.e. family-wise significance of alpha = 0.001) for all structures (Figure 2). IBDM-identified clusters tended to extend beyond the regions of modified doses in the hippocampi and hypothalamus irrespective of whether CT or MRI scans were used, likely due to their location in regions of low dose variability.
Conclusion
CT- and MRI-based IBDM pipelines offer comparable reliability to identify dose-response associations in paediatric brain tumour data. Although MRI offers superior contrast, CT-based IBDM remains a viable option to enable multi-institutional data collection and retrospective studies for late effects research.