Dosimetric beam-angle optimization for non-coplanar dynamic-collimator trajectory radiotherapy
Jenny Bertholet,
Switzerland
OC-0621
Abstract
Dosimetric beam-angle optimization for non-coplanar dynamic-collimator trajectory radiotherapy
Authors: Jenny Bertholet1, Chengchen Zhu1, Silvan Mueller1, Gian Guyer1, Paul-Henry Mackeprang1, Hannes A Loebner1, Werner Volken1, Marco M F Stampanoni2, Daniel M Aebersold1, Michael K Fix1, Peter Manser1
1Inselspital, Bern University Hospital and University of Bern, Division of Medical Radiation Physics and Department of Radiation Oncology, Bern, Switzerland; 2Institute for Biomedical Engineering, ETH Zürich and PSI, Villigen, Switzerland
Show Affiliations
Hide Affiliations
Purpose or Objective
Dynamic-collimator trajectory radiotherapy (colli-DTRT) delivers intensity modulated radiotherapy using multiple non-coplanar partial arcs with dynamic collimator rotation. We solve the beam angle optimization problem for colli-DTRT by determining the table-angle and gantry-angle ranges of the partial arcs through iterative 4pi fluence map optimizations (FMOs) and beam direction elimination.
Material and Methods
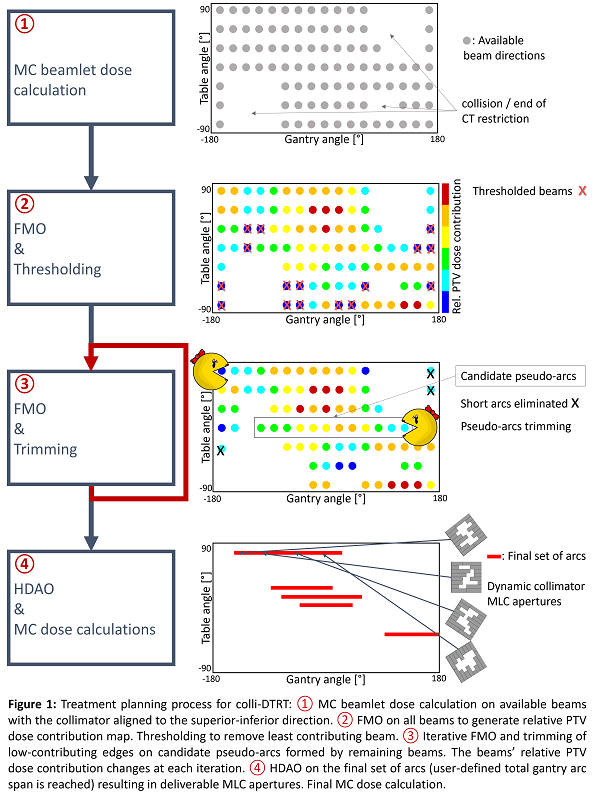
The treatment planning process is shown in figure 1. First, available beam directions are sampled on a gantry-table map and the collimator angle is aligned to the patient superior-inferior axis. In-house Monte Carlo (MC) dose calculation is performed for all beamlets. Second, FMO is carried out on the set of beams to map the relative contribution of each beam direction to the mean PTV dose. The map is thresholded to eliminate the least contributing beams. Third, candidate arcs are formed by remaining adjacent beams with the same table-angle. These are trimmed by iterative FMO and elimination of the least contributing beams at the arcs’ edges. Short candidates are rejected. Step 3 is repeated until the total gantry-angle range reaches a user-defined value. Fourth, the final set of candidates are considered as dynamic arcs for hybrid direct aperture optimization (HDAO) to obtain a deliverable colli-DTRT plan. Final MC dose calculation is performed.
colli-DTRT plans are created for 1 brain (60 Gy to 50% of PTV), 1 lung (66 Gy to 50% of PTV), and 2 head and neck (HN, 50 Gy to 95% of PTV) clinically motivated cases with a total gantry angle range of 720°, and compared to a HDAO-optimized 2 full VMAT arcs plans using the same objectives.
Results
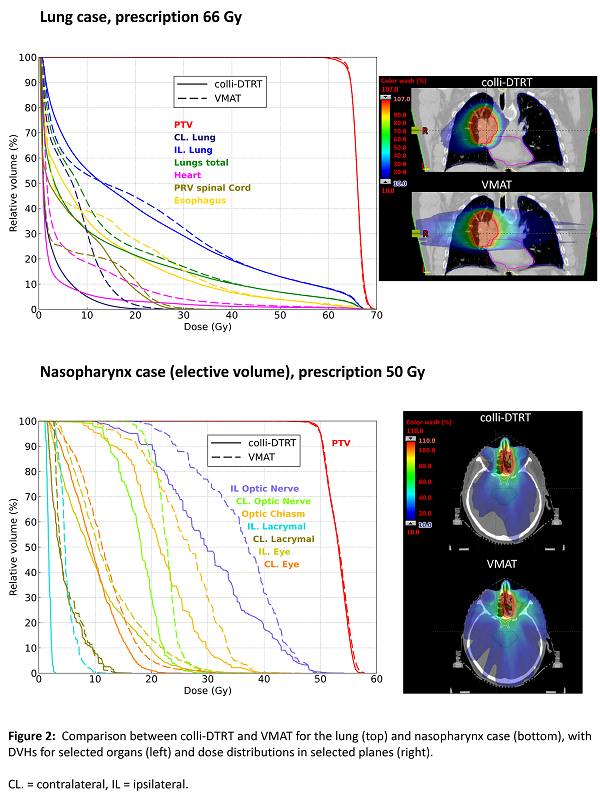
colli-DTRT plans comprised 9-17 partial arcs with a median 50° (min 30°- max 120°) gantry-angle range and table-angles covering the full available range. For the brain case, mean and near-max dose to the brain (excl. PTV) was 1.6 Gy lower, respectively 0.6 Gy higher for colli-DTRT than VMAT. Near-max dose to the brainstem was 55.6 Gy for colli-DTRT and 56.4 Gy for VMAT. For the lung case, the lungs and heart mean doses were on average 2.9 Gy lower for colli-DTRT than for VMAT (figure 2). For an oropharyngeal case (HN1), D5% to the PTV reached 55.2 Gy for VMAT and 53.5 Gy for colli-DTRT. Mean dose to the parotids, oral cavity, pharynx and larynx was on average 2.8 Gy lower for colli-DTRT than VMAT. For a nasopharynx case (HN2), near-max dose to the optic nerves, optic chiasm and eyes was on average 3.0 Gy lower with colli-DTRT than VMAT (figure 2).
Conclusion
We introduced a dosimetrically-motivated approach for beam angle optimization using iterative FMO and beam elimination combined with HDAO to generate deliverable colli-DTRT plans. colli-DTRT was investigated for 4 clinically motivated cases, demonstrating potential to improve organ-at-risk sparing compared to VMAT.
This work was partially supported by Varian Medical Systems and grant 20021_185366 of Swiss National Science Foundation.