Towards simulation-free MR-linac planning for definitive male pelvis treatment
OC-0283
Abstract
Towards simulation-free MR-linac planning for definitive male pelvis treatment
1GenesisCare, Radiation Oncology, Sydney, Australia
Show Affiliations
Hide Affiliations
Purpose or Objective
In the current Elekta Unity MR-Linac (MRL) radiotherapy workflow, a simulation-CT provides reference anatomical and voxelised electron density (ED) information for treatment planning. Each contoured organ is then assigned an average bulk-density value, which is later used to assign densities to structures contoured on the daily MR scans (Figure 1). An MRL provides opportunities to explore novel MR-only workflows [1], which would require accurate ED estimates without simulation-CT [2-4]. This MRL-based study aimed to investigate the dosimetric impact of using an individual- and population-based bulk-density override.
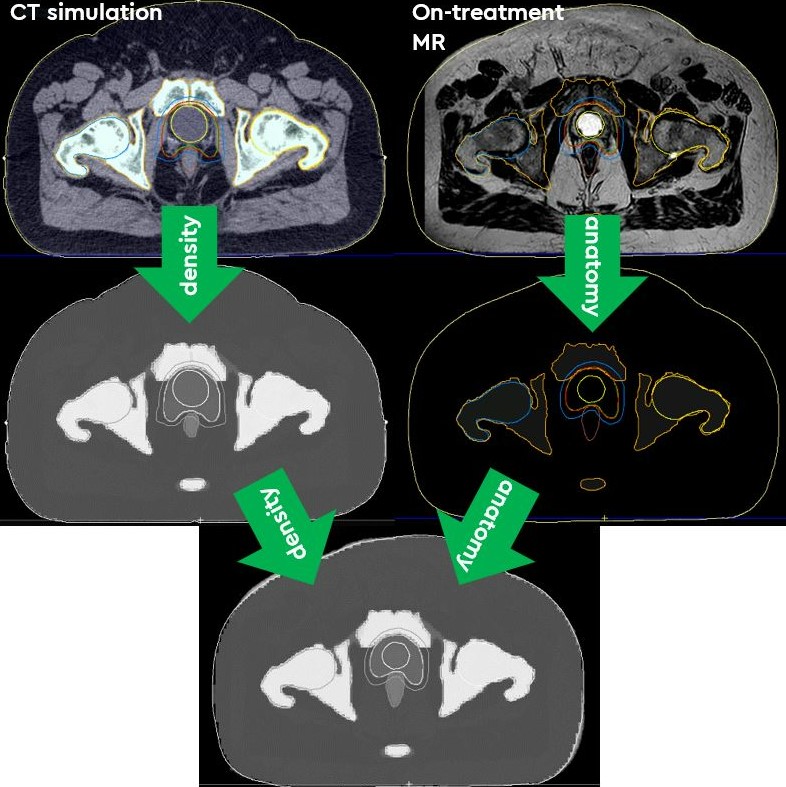
Figure 1. In a standard MRL adaptive workflow, CT simulation data is used to generate the required ED information for each structure. These EDs are then assigned to the contours of the patients’ anatomy, of which are created from the daily on-treatment MR-scan.
Material and Methods
Datasets of 74 male-pelvis patients treated on the St Vincent’s Unity MRL were analysed retrospectively. Their individual-EDs were extracted and the population value was calculated for several organs (bladder, rectum, sigmoid colon, patient outline, bone, femurs and GTV). 10 patients with outlying organ ED values had their reference plans recalculated to find an Individual-ED Dose (IndD) and Population-ED Dose (PopD). Percentage differences in mean dose were calculated between these plans and the voxelised simulation-CT Dose (sCTD).
Results
The individual-EDs of all selected patients remained within 5% of the population average for solid soft tissue organs, and within 8% for bony structures. The largest residual variation was observed for hollow organs (rectum, sigmoid) due to variable amounts of gas included in the contour. The differences in maximum and mean doses, and also in minimum doses for target structures only, between sCTD and IndD/PopD plans remained ≤ ±1.9%, ±2.9% and ±3.7% for soft tissue organs, target organs, and bony structures, respectively. The average of the 10 patients mean dose differences between these noted plans is presented in Figure 2. No clear correlation was observed to occur between structures with larger differences in their individual-ED values compared to the population, and %differences in dose indices between the 3 calculated plans.
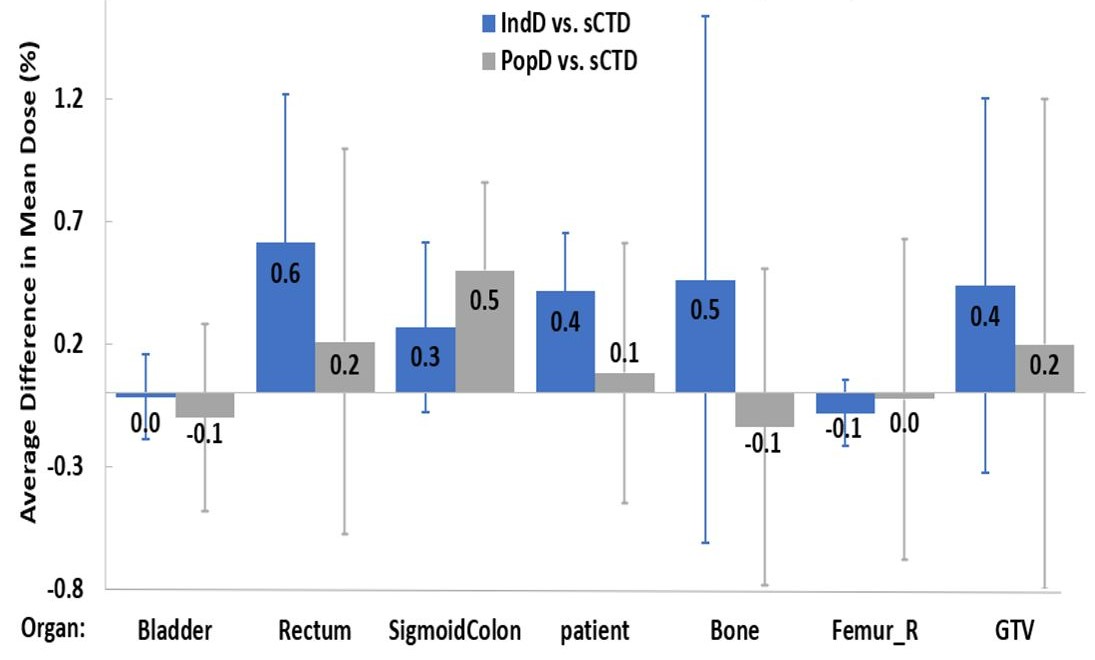
Figure 2. The average of all 10 patients’ percentage difference in mean dose; when calculated between both sCTD and IndD, and sCTD and PopD. The average dose difference calculated for each organ is presented, with error bars representing the standard deviation found between all patients.
Conclusion
Given the comparable dose differences observed between PopD and IndD (current clinical method), using a population-based ED was deemed feasible in an MRL workflow.
References:
- Lui et al. Precis Radiat Oncol. 2022; 6:75-84
- Karotki et al. J Appl Clin Med Phys. 2011;12:97-104
- Hsu et al. Phys Med Biol. 2018;63:155003
- Prior et al. Phys Med Biol. 2016;61:3819-3842