TOAST Classification of Ischemic Stroke in NPC Post-Radiotherapy: A Nationwide Cohort Study
PD-0402
Abstract
TOAST Classification of Ischemic Stroke in NPC Post-Radiotherapy: A Nationwide Cohort Study
Authors: Ting-Chun Lin1,3, Chin-Yang Lin2, Cheng-Li Lin4,5, Yo-Liang Lai1
1China Medical University Hospital, Department of Radiation Oncology, Taichung, Taiwan; 2China Medical University Hospital, Department of Neurology, Taichung, Taiwan; 3China Medical University, Graduate Institute of Biomedical Sciences, Taichung, Taiwan; 4China Medical University Hospital, Management Office for Health Data, Taichung, Taiwan; 5China Medical University, College of Medicine, Taichung, Taiwan
Show Affiliations
Hide Affiliations
Purpose or Objective
The standard treatment of nasopharyngeal carcinoma (NPC) is definitive radiotherapy (RT) with or without chemotherapy. Radiotherapy to the neck is known to cause ischemic stroke, and the underlying cause of RT-induced stroke is generally accepted as post-irradiation vasculopathy, leading to arterial stenosis and plaque formation. Although the associated risk factors of ischemic stroke in head and neck cancer have been frequently discussed in multiple studies, the pattern and type of post-RT stroke is rarely examined.
The prognosis and outcome of ischemic stroke is strongly linked to its etiology, and patients receive treatment based on their individual ischemic stroke mechanism. According to Trial of ORG 10172 in Acute Stroke Treatment (TOAST) classification, ischemic stroke can be classified into five categories based on its etiology: large‐artery atherosclerosis, small vessel occlusion, cardioembolism, stroke of other determined etiology, and stroke of undetermined etiology.
In this study, we report the TOAST classification of ischemic stroke in NPC patients by combining the multicenter cancer registry database and the stroke registry database in Taiwan. By analyzing the nationwide databases, we provide the real-world data of stroke characteristics in post-RT NPC patients.
Material and Methods
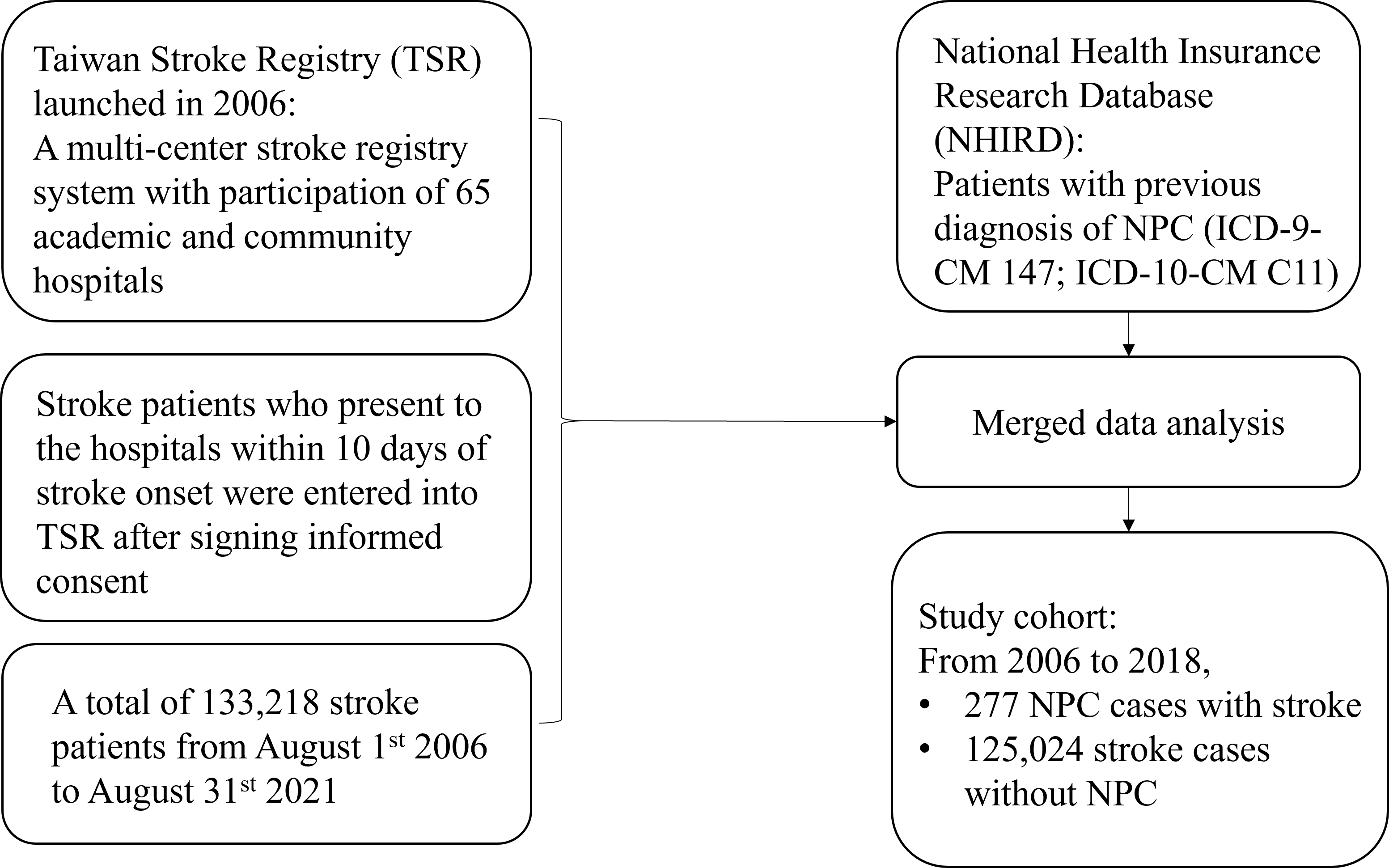
We included patients with stroke from the Taiwan Stroke Registry (TSR) from 2006 to 2018. Patients with a previous diagnosis of NPC (ICD-9-CM 147; ICD-10-CM C11) were identified from the National Health Insurance Research Database (NHIRD). The NHIRD and TSR databases were linked by encrypted and unique personal identification numbers. We therefore identified stroke patients with a history of NPC as our study cohort and further established a comparison cohort comprising stroke patients without NPC.
Figure 1. Flow diagram of study cohort design
Results
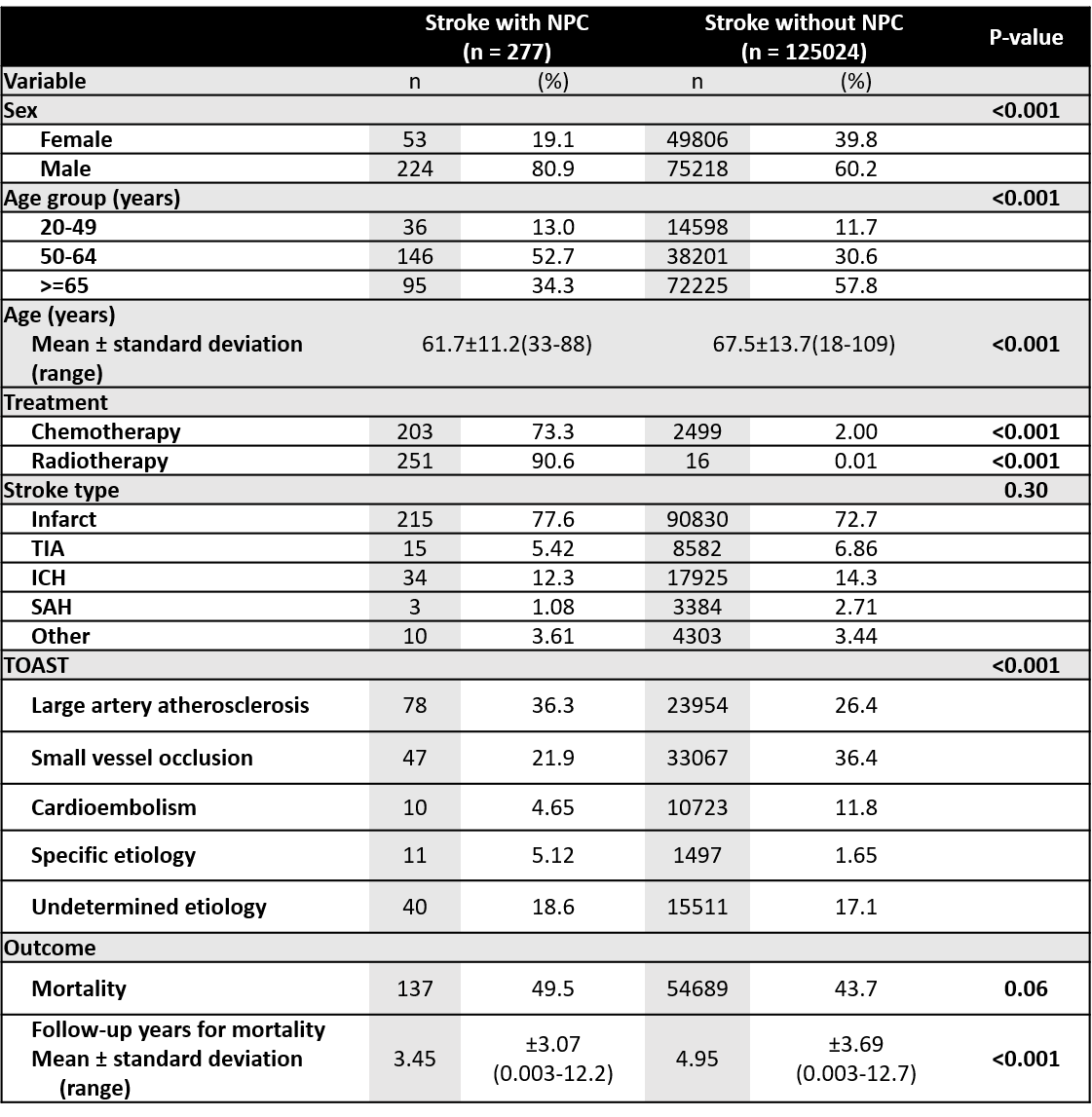
From year 2009 to 2018 in Taiwan, a total of 277 NPC patients with subsequent stroke were identified. The average age of stroke patients with NPC was 61.7 years old. Male predominance was observed (F:M = 1:4). The main type of stroke was infraction (77.6%), followed by transient ischemic attack (TIA), intracerebral hemorrhage (ICH) and subarachnoid hemorrhage (SAH), which was not distributed differently from stroke patients without NPC. The TOAST classification of post-RT ischemic stroke in NPC patients revealed large artery atherosclerosis as the primary etiology, which was statistically higher compared to stroke patients without NPC (36.3% and 26.4%, respectively; P-value < 0.001). The area of infarction (anterior or posterior circulation) was not statistically different between NPC and non-NPC stroke patients.
Table 1. Cohort characteristics
Conclusion
We discovered a 10% statistically significant increase in large artery atherosclerosis as the main etiology of ischemic stroke in NPC patients based on the nationwide database analysis. This study may help physicians more accurately evaluate the risk and treatment of ischemic stroke in NPC patients.