The effect of dose to the brain on early self-reported neurocognition; does low dose matter?
Femke Vaassen,
The Netherlands
PD-0401
Abstract
The effect of dose to the brain on early self-reported neurocognition; does low dose matter?
Authors: Femke Vaassen1, David Hofstede1, Catharina M.L. Zegers1, Jeanette B. Dijkstra2, Frank Hoebers1, Inge Compter1, Wouter van Elmpt1, Daniëlle B.P. Eekers1
1Maastricht University Medical Centre+, GROW School for Oncology and Reproduction, Department of Radiation Oncology (Maastro), Maastricht, The Netherlands; 2Maastricht University Medical Centre+, Department of Medical Psychology, Maastricht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
To evaluate early cognitive deterioration following radiotherapy (RT) for brain and head-and-neck (HN) tumors, extensive cognitive testing before and after treatment is optimal, but also demanding and time-consuming. Patient-reported outcomes (PROMS) are already validated and widely implemented in clinical practice worldwide. As such, this retrospective study aimed to determine if evaluating PROMS on cognitive function could be an alternative to extensive cognitive tests and to determine if there is a dose-effect relation to neuro organ-at-risk (OARs).
Material and Methods
105 brain and 260 HN patients treated with RT between 2012-2021 were included. PROMS data were collected at baseline and one-year follow-up after RT. Questions relating to cognition from the QLQ-C30 questionnaire (Q20 and Q25) were included. The original four-point scale scores on both questions were combined and transformed to a 100-point cognitive functioning scale. For 12 patients, missing baseline and one-year follow-up data was observed for one question. A strong correlation between each question singularly and cognitive functioning scale (r>0.94, p<0.001) allowed for imputation of the total scale to be based on one answered question. Per patient, the change in cognitive score (ΔCS) was determined from baseline to one-year follow-up and assigned to one of three subgroups (improvement, constant or deterioration). Mean doses (Dmean) were evaluated for the brain, brainstem, supratentorial brain, cerebellum (whole, anterior and posterior) and hippocampus (left and right). A combination of Mann-Whitney U-test and Chi2-test were used to analyze the PROMS data. The relationship between OAR dose and ΔCS was investigated using Kruskal-Wallis tests.
Results
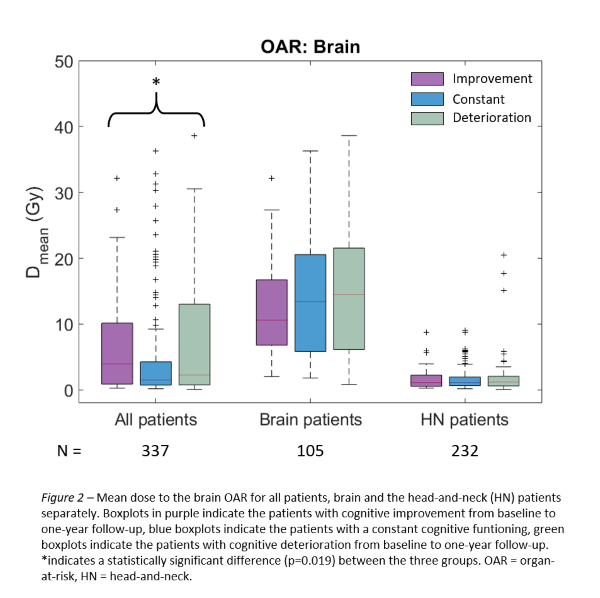
Cognitive scores at baseline and one-year follow-up were significantly lower for brain compared to HN patients (p<0.001) whilst ΔCS showed no significant difference. The majority of HN patients (61%) showed no change in their cognitive score at one-year after RT (see Figure 1). Although the HN patients received only low doses to the OARs, with the cerebellum receiving the highest mean dose of 5.5 Gy, 28% of them showed deterioration in their cognitive score at one-year after RT. More brain patients had a cognitive deterioration compared to HN patients (44% vs 28%, p=0.001). Age <65 years was associated with cognitive deterioration (p=0.025). More female patients had a cognitive deterioration at one-year after RT compared to male patients (37% vs 31%, p=0.02). There is a significant relationship between the mean dose to the brain and ΔCS (p=0.019, Figure 2). No significant correlation was observed for the other OARs.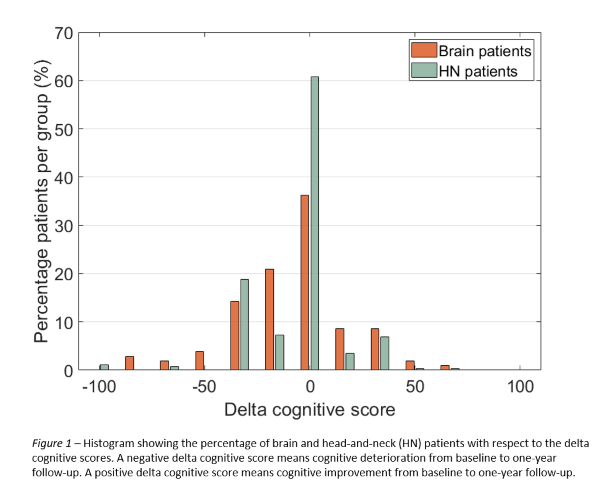
Conclusion
A significant difference in baseline and one-year follow-up cognitive scores was found between brain and HN patients. The mean brain dose, treatment location, sex and age were associated with cognitive performance after RT. Future research includes adding baseline WHO performance status, tumor type and more dose parameters on this dataset.