Clinical outcome of lung-only oligometastatic HNSCC patients treated with SBRT: Update results
PD-0397
Abstract
Clinical outcome of lung-only oligometastatic HNSCC patients treated with SBRT: Update results
Authors: Viola Salvestrini1, Ilaria Bonaparte2, Niccolò Bertini3, Chiara Mattioli3, Chiara Bellini3, Carlotta Becherini3, Isacco Desideri3, Pietro Garlatti3, Marco Banini3, Ludovica Zisca3, Lorenzo Livi3, Pierluigi Bonomo3
1CyberKnife Center, Istituto Fiorentino di Cura ed Assistenza, Radiation Oncology, Florence, Italy; 2Azienda Ospedaliero Universitaria Careggi, University of Florence, Radiation Oncology, Florence, Italy; 3Azienda Ospedaliero-Universitaria Careggi; University of Florence, Radiation Oncology, Florence, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Oligometastatic disease in head and neck squamous cell carcinoma (HNSCC) is an atypical scenario. Local ablative treatments are the most adopted strategies although no evidence-based recommendations are currently available. The purpose of our analysis was to update and report on long-term clinical outcomes of a cohort of HNSCC patients treated with stereotactic body radiotherapy (SBRT) for lung-only oligometastatic disease.
Material and Methods
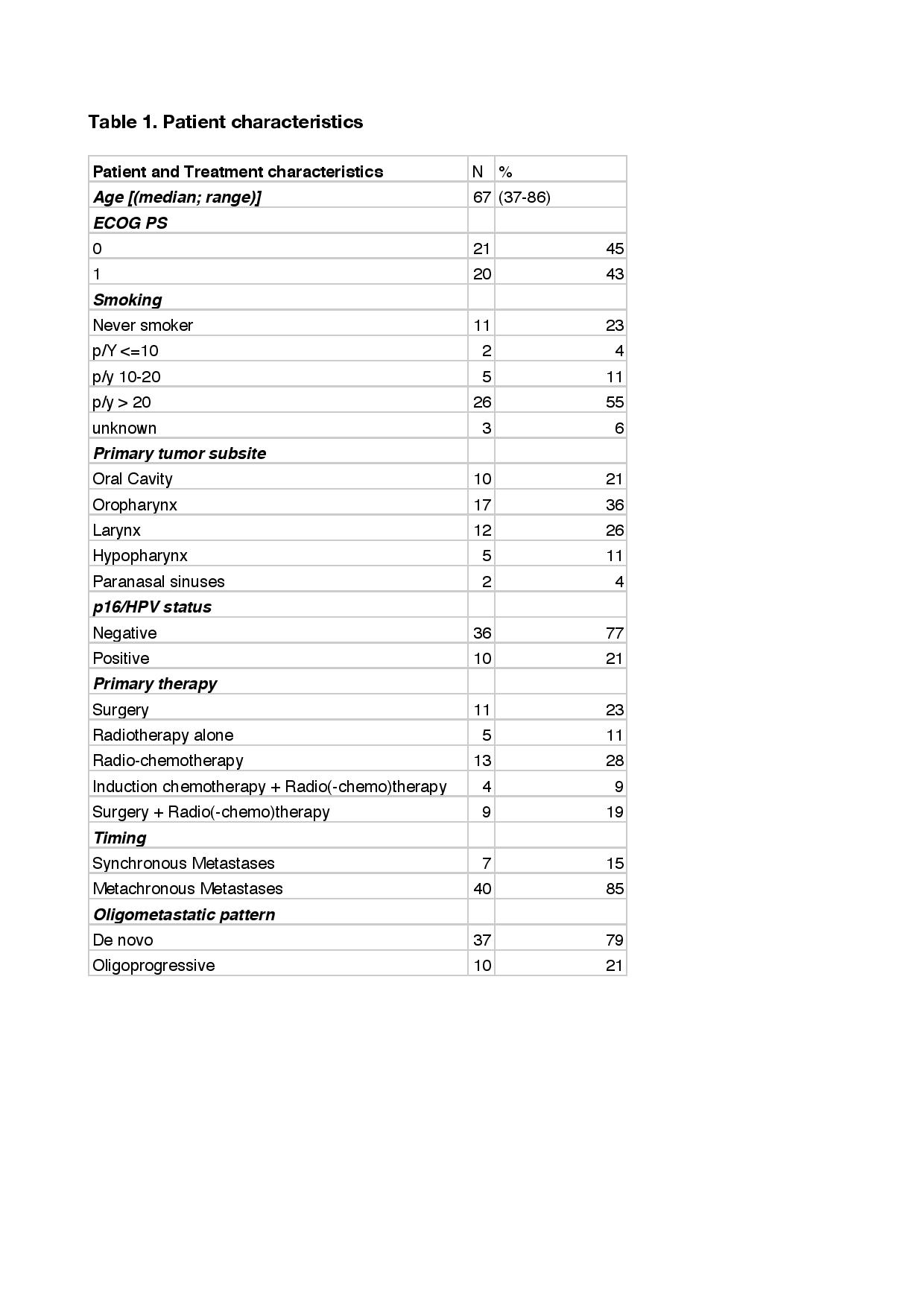
We included patients with 1 to 5 pulmonary lesions. The oligometastatic pattern was defined as “de novo” (suitable for SBRT only) or “oligoprogressive” (after first line of systemic therapy). We evaluated time to progression (TTP) as the time from the last day of SBRT to disease progression or death from any cause. Predictive factors of better clinical outcome and survival analysis were performed by Cox regression and Kaplan Meier methods, respectively.
Results
A cohort of 47 patients and 48 metastases were retrospectively evaluated (Table 1). The median age was 67 years (range 37-86) and 87% of patients had a ECOG PS 0-1. HPV negative status (77%) and “de novo” oligometastatic pattern (78%) were reported by the majority of patients. After a median follow up of 28 months (range 2-88), median TTP and overall survival (OS) were 18 months (95% CI 4.8 – 31.2) and 62 months (95%CI 10,8 - 113.2), respectively (Figure 1). At univariate analysis, patients aged > 70 years reported a better TTP (p 0.013). No statistically significant correlation was observed in respect with gender (p 0.23), ECOG PS (p 0.34), oligometastatic pattern (p 0.13) and p16/HPV status (p 0.22). Out of 26 histologically proven metastases, we collected only 2 patients reporting concordance between p16/HPV positive status of primary tumor and lung metastases. Overall, 6 patients reported grade (G) 1-2 acute toxicity and no acute G3 adverse events were observed.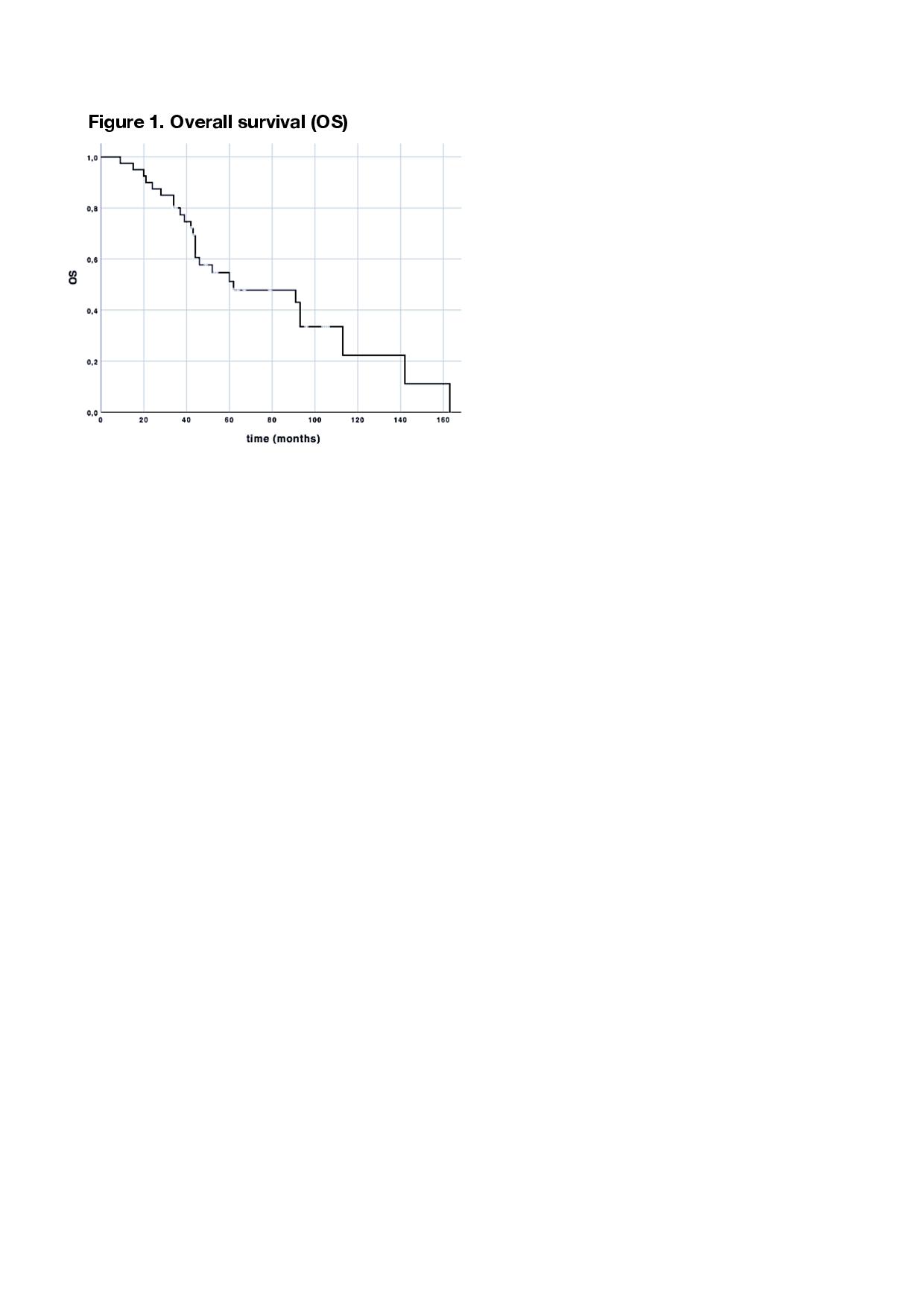
Conclusion
In appropriately selected HNSCC patients with lung-only oligometastatic disease, SBRT may improve clinical outcome prolonging time to progression and to systemic treatments. Distant metastases from HPV-related primary HNSCC should be tested for p16/HPV status given the clinical implications of HPV positivity for diagnosis and treatment.