Guidance for simulation to enhance education of pre-registration Therapeutic Radiographers
Nicky Hutton,
United Kingdom
PD-0734
Abstract
Guidance for simulation to enhance education of pre-registration Therapeutic Radiographers
Authors: Nicky Hutton1, Sarah-Jane Ketterer1
1Society and College of Radiographers, Professional and Education, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Simulation has been shown to have a positive effect on knowledge, skills, confidence, and patient-related outcomes(1). Over the past decade there has been increased interest in the use of simulation as educators seek to optimise student experience and ensure placement opportunities can be utilised effectively and efficiently.
There is a national drive to develop simulation, so that it is equitably available to all pre-registration students and staff, so that the future workforce can meet the demands of providing safe and effective care (2).
This modified Delphi research method has enabled the Society of Radiographers to elicit consensus opinion on priority areas for simulation within the Radiotherapy curriculum, and develop national guidance.
Material and Methods
A multi-stage mixed method approach was undertaken, guided by a project steering group.
1. Initial scoping survey across UK HEIs delivering pre-registration Health and Care Professions Council (HCPC) approved Therapeutic Radiography programmes of education n=14, to determine current provision for simulation.
2. A consensus study using a modified Delphi research methodology across UK HEIs n=14, UK NHS radiotherapy clinical healthcare providers n=59 and UK private radiotherapy providers n=15 to gather consensus opinion on the priority areas for simulation within pre-registration education and training of therapeutic radiographers.
3. Dual moderator focus groups with key stakeholders including SoR Patient Advisory Group (PAG) representatives n=4 and SoR student member representatives n=4.
Results
Recommendations
1. HEIs and clinical placement providers should seek to align simulation activities with programme learning outcomes and the HCPC Standards of Proficiency.
2. Partnership working between each HEI and their local clinical placement providers will provide maximum impact, allowing local decisions to be made regarding how simulation can be best utilised within programmes.
3. Simulation activities should align to a process model and include briefing and debriefing to support good quality simulation and achievement of learning outcomes.
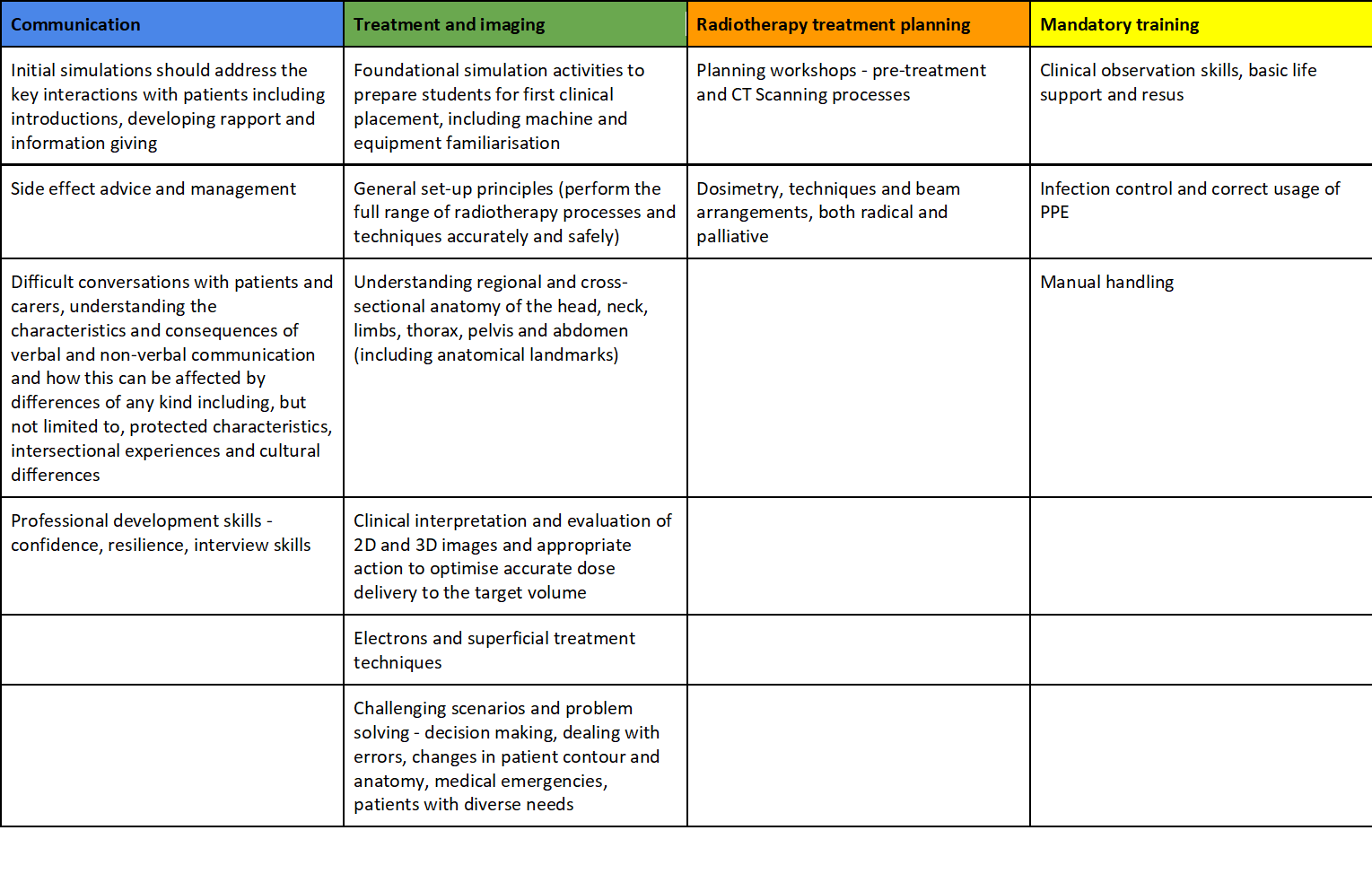
4. There are four overarching themes where educators should focus simulation efforts to ensure maximum gain for student learning and experience (see table 1.).
Both Patient Advisory Group and student member focus groups identified a number of priority simulation activities which aligned with those identified in the Delphi study. The key areas were communication and confidence, which affects both student confidence levels and patient experience.
Table 1.
Conclusion
This multi-stage, mixed method research approach has identified key recommendations for the use of simulation in enhancing pre-registration education and training of Therapeutic Radiographers. It has also provided robust evidence for the priority areas within the radiotherapy curriculum that could provide the most benefit when delivered via simulation; this is supported by multi professional case studies.