Association of Statin Intensity With Cardiac Events and Mortality After Radiotherapy for NSCLC
PD-0159
Abstract
Association of Statin Intensity With Cardiac Events and Mortality After Radiotherapy for NSCLC
Authors: Gerard Walls1, John O'Connor1, Eamon McCarron2, Valentina Giacometti3, Frances Duane4, Mark Harbinson5, Conor McCann5, Peter McKavanagh5, Anna Gavan6, Jonathan McAleese3, Aidan Cole3, Karl Butterworth1, Conor McGarry3, Gerry Hanna1, Suneil Jain1
1Queen's University Belfast, Patrick G Johnston Centre for Cancer Research, Belfast, United Kingdom; 2Belfast Health & Social Care Trust, Department of Clinical Biochemistry, Belfast, United Kingdom; 3Belfast Health & Social Care Trust, Northern Ireland Cancer Centre, Belfast, United Kingdom; 4St Luke’s Radiation Oncology Network, Department of Radiation Oncology, Dublin, Ireland; 5Belfast Health & Social Care Trust, Department of Cardiology, Belfast, United Kingdom; 6Queen's University Belfast, Northern Ireland Cancer Registry, Belfast, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Mechanisms by which cardiac radiation dose leads to death are purported to include acute cardiac events and subclinical impairment of cardiac function that impedes recovery from other acute medical issues. Whilst historically prescribed to lower serum lipids, cardiology guidelines now recommend statins for a myriad of cardiovascular risk factors (CVRFs), owing to their anti-inflammatory, antifibrotic and antioxidant properties. Herein the association of statin intensity with survival in patients completing NSCLC radiotherapy (RT) is examined.
Material and Methods
Patients treated with curative-intent RT between 2015-2020 at a regional centre were identified. Clinical notes were interrogated for baseline patient, tumour and CVRF details and both follow-up cancer control and CV events. The latter were verified by a cardiologist. Death certificates were accessed for the primary cause of death. RT planning scans were retrieved for application of a deep learning-based auto-segmentation tool to generate cardiac chamber and great vessel structures. The coronary arteries and conduction nodes were added manually and the former were verified by the atlas lead author. A composite cardiac base structure was created. All plans were re-calculated with the same AAA algorithm. Three Cox proportional hazards regression models for overall survival were generated: unadjusted, adjusted for tumour factors and CVRFs only, and a model fully adjusted with all of the available parameters including previous cardiac events.
Results
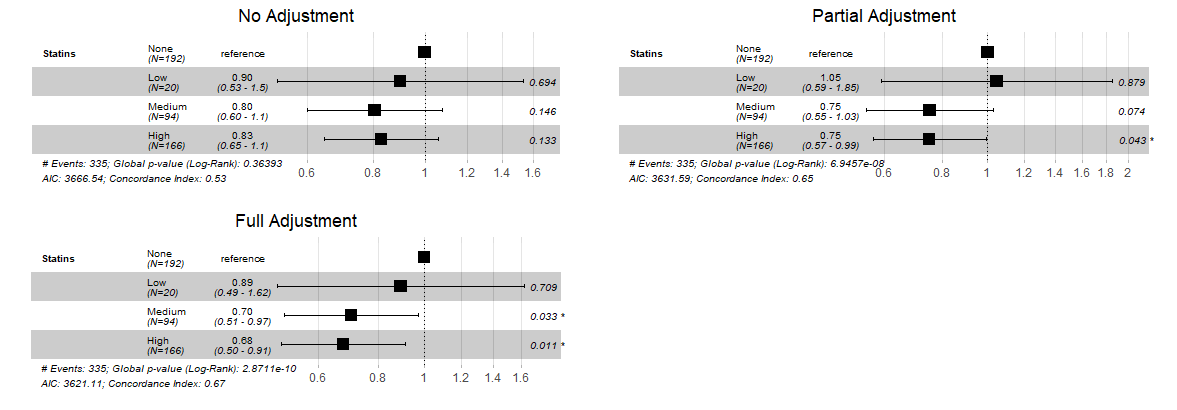
A total of 478 patients were included, with a median age of 70, Charlson Comorbidity Index of 5 and BMI of 26.5. The median heart base dose was 9.6Gy (IQR 5.5–15.1Gy). The median lung V20 was 20.0% (IQR 14.8–27.1). CVRFs were common, with most patients having 2 (39%) or 3 (31%). The median QRISK3 score was 18.7. A low (4%), medium (20%) and high (35%) dose statin was prescribed to 4%, 20% and 35% patients. Acute cardiac events occurred in 79 patients across the no statin (15%) and low (15%), medium (17%) and high (18%) dose groups. There was no significant difference in time to locoregional (p=0.25) or distant (p=0.25) disease progression. In the fully adjusted regression models for overall survival, low (HR 0.89, p=0.71), medium (HR 0.70, p=0.03) and high (HR 0.68, p=0.01) intensity statin therapy were associated with reduced mortality. These hazard ratios were similar to the partially adjusted model as shown in the Forest plots (Figure 1).
Conclusion
These data represent the first evidence that statin intensity is associated with reduced mortality in patients receiving curative-radiotherapy for NSCLC. Pre-planned model adjustments suggest CVRFs have a considerable impact on survival. Neither the prevalence of cardiac events nor locoregional or distant control were affected by statin intensity. We hypothesise that statin therapy may mitigate subclinical radiation cardiac damage, increasing the probability of surviving acute medical issues.