Prostate radiotherapy may cause fertility issues – analysis of testicular dose following modern RT
PD-0568
Abstract
Prostate radiotherapy may cause fertility issues – analysis of testicular dose following modern RT
Authors: Manon KISSEL1, Mario TERLIZZI1, Nicolas GIRAUD2, Anthony ALEXIS3, Marjolaine CHEVE3, Julien VAUTIER3, Alberto BOSSI1, Phillippe MORICE4, Pierre BLANCHARD1
1Gustave Roussy, Radiotherapy, VILLEJUIF, France; 2CHU Bordeaux, Radiotherapy, BORDEAUX, France; 3Gustave Roussy, Radiophysics, VILLEJUIF, France; 4Gustave Roussy, Gynecologic surgery, VILLEJUIF, France
Show Affiliations
Hide Affiliations
Purpose or Objective
Prostate cancer in younger men is not infrequent. Radiotherapy is a cornerstone of prostate cancer treatment and yet, its impact on fertility is scarcely reported in literature. Since testis is one of the most radiosensitive tissue, we tried to determine testicular dose with modern radiotherapy techniques for a definitive prostate irradiation.
Material and Methods
One hundred radiotherapy plans were reviewed. Testicles were contoured a posteriori without any optimization on testicles.
Results
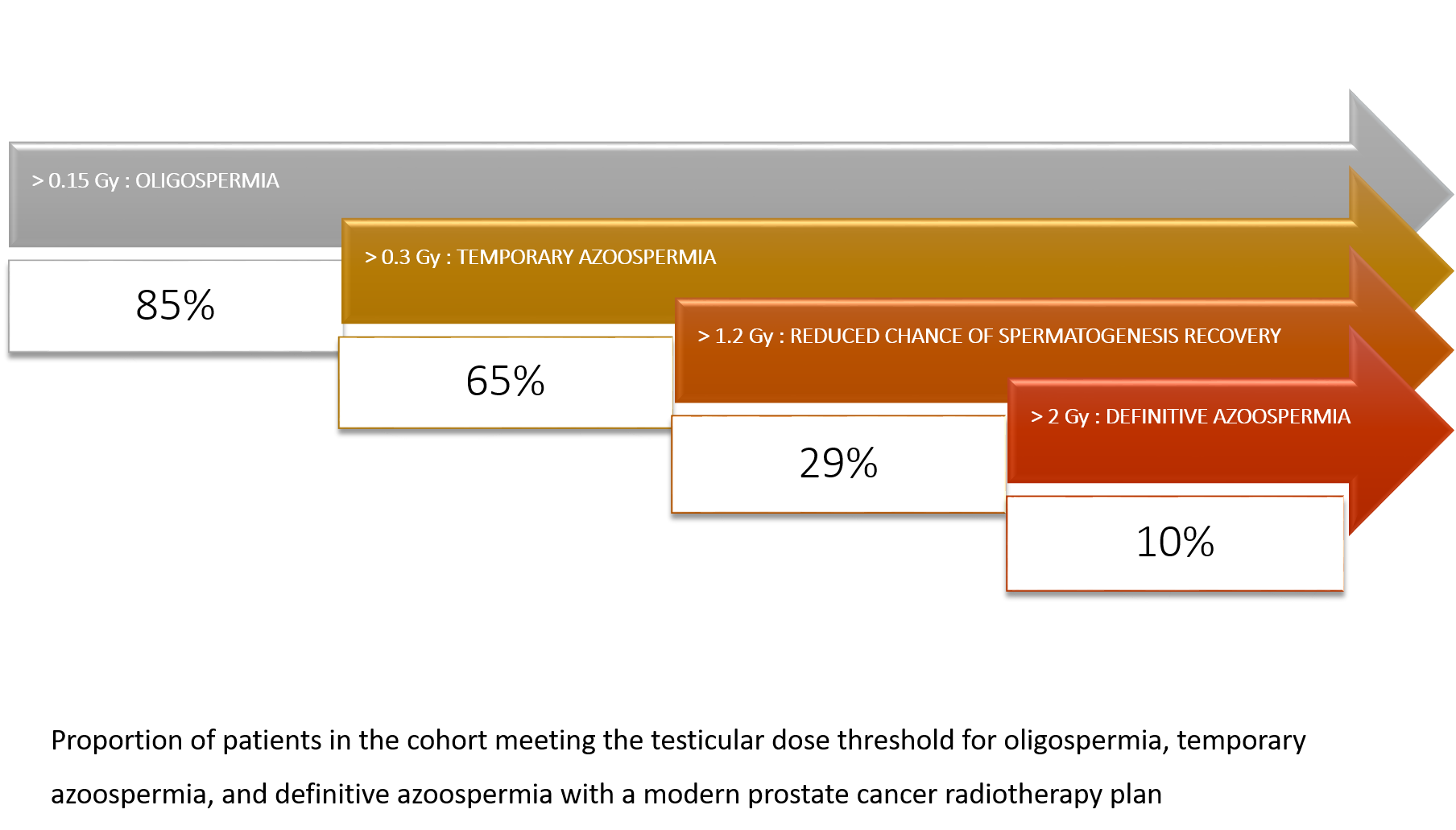
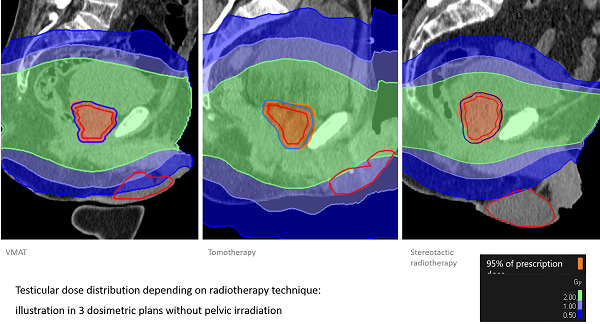
Median testicular dose was 0.58 Gy: 0.18 Gy in stereotactic plans versus 0.62 Gy in Volumetric Modulated Arc Therapy plans versus 1.50 Gy in Tomotherapy plans (p < 0.001). Pelvic nodal irradiation increased the median testicular dose: 1.18 Gy versus 0.26 Gy (p < 0.001). Weight and BMI were inversely associated with testicular dose (p < 0.005). 65% of the patients reached the theoretical dose threshold to get transitory azoospermia and 10% received more than 2 Gy, that is likely to give definitive azoospermia.
Conclusion
Although probably lower than what used to be delivered with older techniques, testicular dose delivered with modern prostate radiotherapy is not negligible and is often underestimated because the contribution of daily repositioning imaging is not taken into account and most Treatment Planning Systems underestimate the out of field dose. Radiation oncologists should be aware of the possible impact of prostate radiotherapy on fertility and gonadal endocrine secretion. Men should be counselled at first consult and offered a sperm preservation strategy if they have a paternity wish.