HDR brachytherapy for Cervical Cancer: Evolving anaesthetic technique to improve patient experience
Stephanie Brown,
United Kingdom
PD-0407
Abstract
HDR brachytherapy for Cervical Cancer: Evolving anaesthetic technique to improve patient experience
Authors: deborah gregory1, Tracy Christmas2, Sarah Prewett1, Katie Bradshaw1, John Latimer3, Simon Duke1, Li Tee Tan1
1Cambridge University Hospitals, Clinical Oncology, cambridge, United Kingdom; 2Cambridge University Hospitals, Anaesthesia, cambridge, United Kingdom; 3Cambridge University Hospitals, Gynaecology, cambridge, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
The use of intra-cavity applicators, particularly interstitial implants to deliver HDR brachytherapy for cervical cancer is consistently associated with high levels of pain. 41% of patients experience PTSD at 3 months. In our institution BT is delivered with one applicator insertion, with 3 or 4 fractions delivered over 3 days. Typically insertions were under GA with epidural in the post operative period. We noted that under continuous epidural analgesia pain scores for women were high whilst the applicator remained in situ and numerous pain interventions were required. Following the appointment of a regular brachytherapy anaesthetist we changed practice to a combined spinal-epidural with intrathecal diamorphine to provide anaesthesia for insertion and post-insertion analgesia with epidural analgesia. A retrospective review of cases over a 5 year period evaluated the impact of this intervention.
Material and Methods
In the study period combined spinal-epidural (CSE) anaesthesia was the preferred technique for applicator insertion. In the first 12 months this was supplemented with a general anaesthetic (GA), subsequently awake insertion was undertaken. The intrathecal component comprised 10 mg hyperbaric bupivacaine and 500 mcg diamorphine. Analgesia was maintained post-insertion with a continuous epidural infusion of 0.1% levobupivacaine and 2 mcg/ml fentanyl titrated to effect. Where regional anaesthesia was contraindicated GA was performed and post-insertion pain relief maintained with patient-controlled intravenous analgesia (PCA) using primarily oxycodone. Pain scores were recorded in recovery and at intervals post insertion. The total number of interventions by the pain team were noted. Other anaesthetists were encouraged to use a similar technique.
Results
108 women underwent 121 insertions, 62% of procedures were anaesthetised by TC, the remainder were performed by 31 different senior anaesthetists, choice of technique was dependent on the anaesthetist’s personal choice/clinical situation.
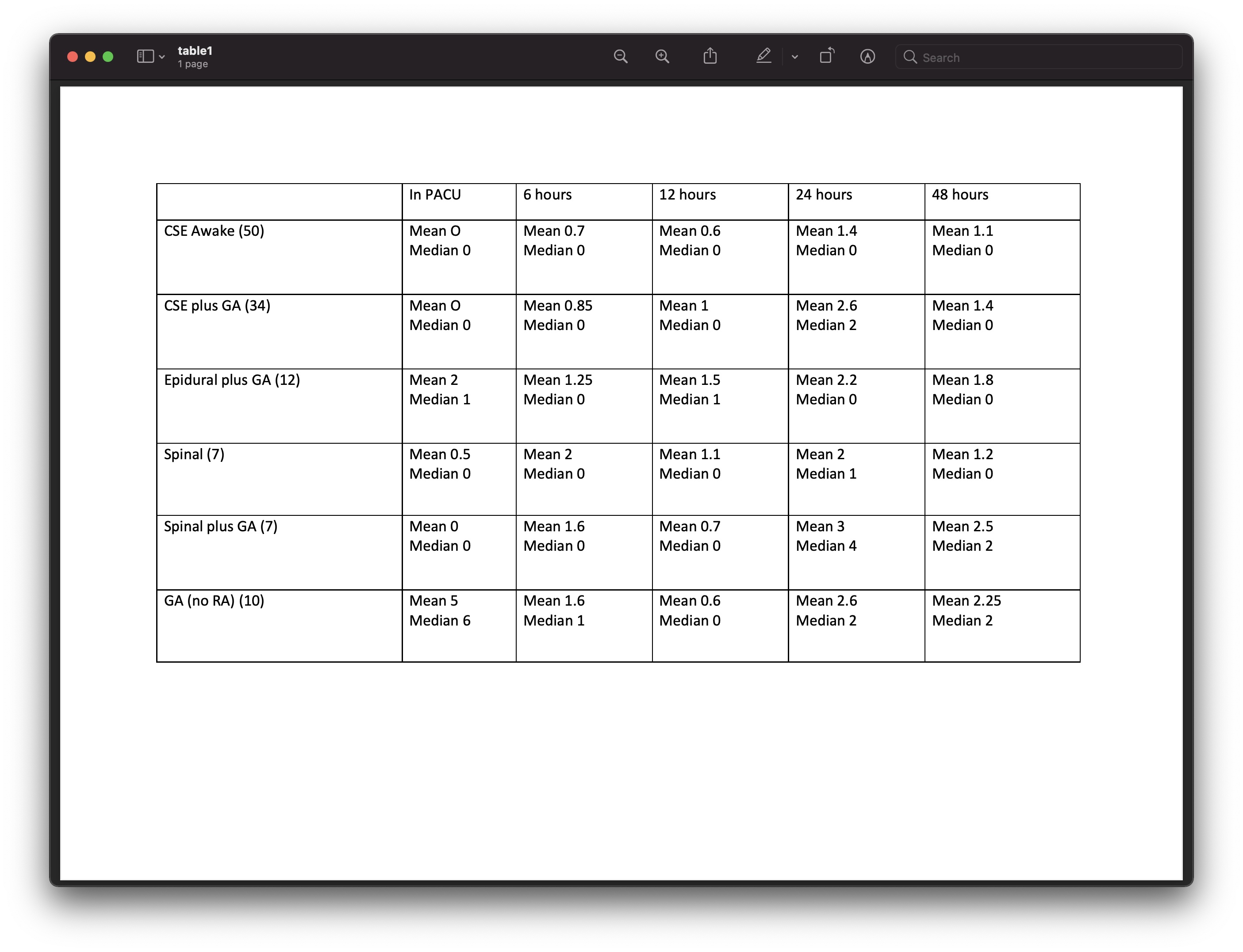
Pain scores are shown in Table 1. The highest pain scores were in those patients in whom a GA was used with no regional anaesthesia; pain scores improved with PCA. 46 insertions required no additional pain interventions in the postoperative period. 19 cases required 3 or more post-operative interventions above the routine acute pain daily ward round: 15 CSEs (18% of all CSEs performed), 3 epidurals (25%) and 1 spinal (7%).
Conclusion
The CSE technique provides comparable analgesia to other forms of neuraxial block, reduces post-operative pain interventions compared to epidural analgesia alone. A positive unexpected consequence of this change in practice was the possibility for awake insertions which accelerated the recovery process, permitting more rapid delivery of the first fraction, improving safety by reducing the rate of out of hours treatment