Which cervical cancer patients need adaptive planning? A new approach to predicting target motion
PD-0740
Abstract
Which cervical cancer patients need adaptive planning? A new approach to predicting target motion
Authors: Lei Wang1, Sarah Mason2, Dualta McQuaid1, Matthew Blackledge2, Helen McNair1, Emma Harris2, Susan Lalondrelle3
1Royal Marsden Hospital NHS Trust, Radiotherapy department, Sutton, United Kingdom; 2Institute of Cancer Research, Department of Radiotherapy and Imaging, Sutton, United Kingdom; 3Royal Marsden Hospital NHS Trust and Institute of Cancer Research, Department of Radiotherapy and Imaging, Sutton, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Target motion during cervix cancer radiotherapy can lead to geographic miss. Use of an internal target volume (ITV) for the low-risk clinical target volume (CTV-LR) based on full and empty-bladder CTs (CT-FB and CT-EB) can model the range of motion of a specific patient. However, this often fails to predict target position during treatment. Patients may be termed “movers” if the uterine fundus tip at planning moves over an arbitrary threshold between CT-FB and CT-EB: such cases can be highlighted for adaptive techniques such as plan-of-the-day. However, some non-movers at planning become movers at treatment. A method to identify these "occult movers" is lacking. We analysed planning CT features and patient demographics to identify markers of occult movers pre-treatment.
Material and Methods
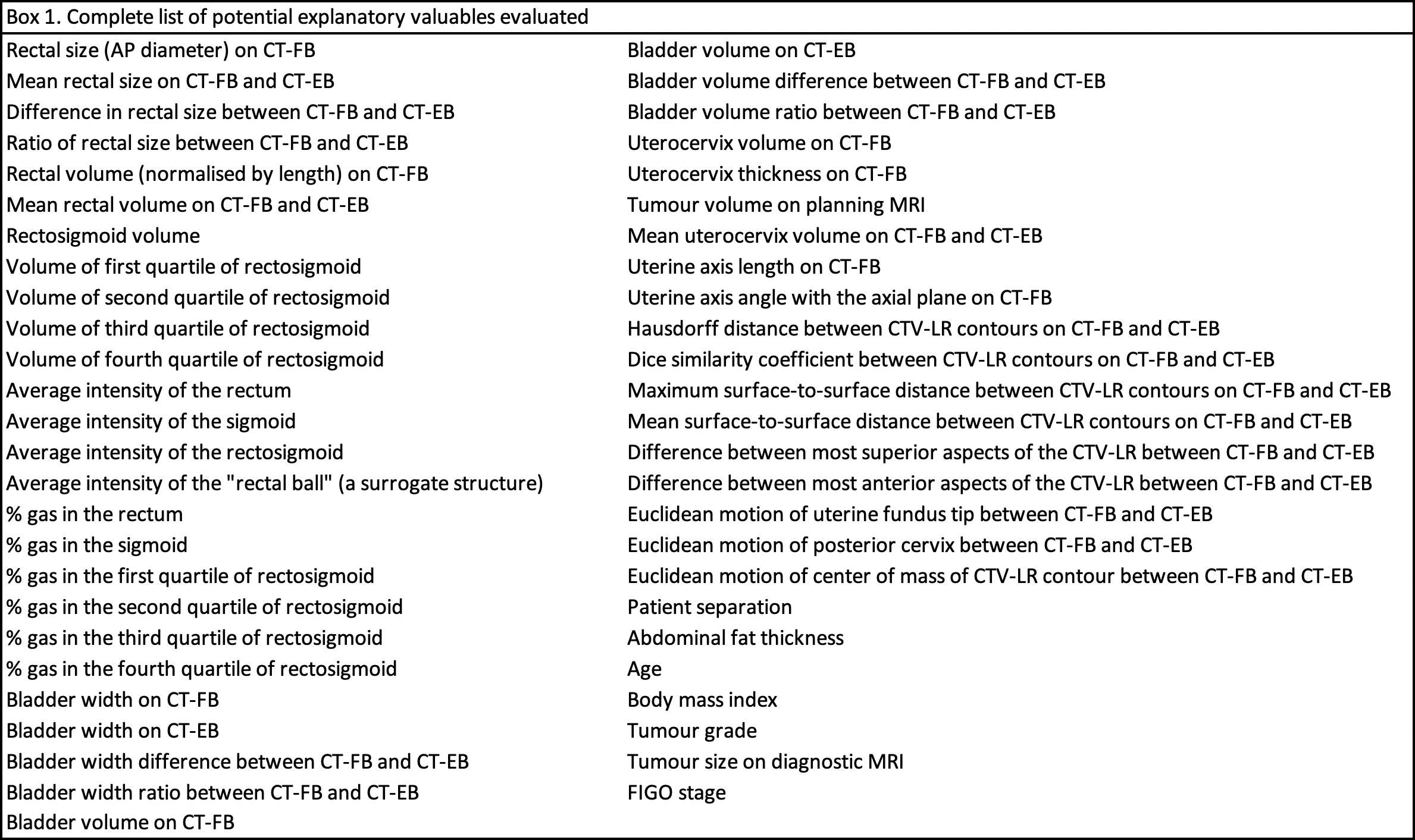
160 images from 20 cervix cancer patients were evaluated. For each, CT-FB, CT-EB, planning MRI and 5 randomly chosen cone-beam CTs were contoured (CTV-LR, bladder, rectum) following the EMBRACE-II protocol. ITVs were created by interpolating between CT-EB and CT-FB CTV-LR contours and expanded by 7 mm to create a planning target volume (PTV). The MRI was ignored for ITV creation and treated as another fraction. A patient was designated "covered" if the CTV-LR was >95% covered in 5/6 fractions and the CTV-HR (tumour and cervix) in 6/6 fractions. Potential explanatory variables (EVs) included various measures of organ shape, and contents on planning CT (Box 1) plus age, BMI, tumour grade and FIGO stage.
Prior to model development, 4 patients were removed at random.
Step 1: We analysed EVs individually for ability to predict coverage; the best performing in each category were combined in a logistic regression model, adjusted to achieve the highest mean accuracy in the validation set using 10-fold cross validation (random shuffle of training (n=11) and validation (n=5) sets).
Step 2: Model coefficients were determined on the 16-patient training set.
Step 3: The final model was tested on 4 unseen patients.
Results
Step 1: The chosen EVs (rectal size on CT-FB, bladder width on CT-FB, max surface-to-surface distance between CTV-LR contours on CT-FB and CT-EB, and menopausal status) had 78% average accuracy (s.d. 17%) and 86% average specificity in the cross-validation.
Step 2: The coefficients were -0.68, 0.47, 0.90, 0.70, the intercept was -0.75. When applied to the training set (n=16) the model had 87.5% accuracy, 80% sensitivity, 91% specificity.
Step 3: When applied to the unseen test set (n=4) the model had 75% accuracy, 67% sensitivity and 100% specificity (one patient with adequate coverage was mis-classified as an occult mover). Overall, 8/20 patients were covered (6 in the training set, 2 in the test set).
Conclusion
Using 4 EVs, our model predicted with 75% accuracy and 100% specificity whether a patient’s interfractional motion will fall within the range on CT-EB and CT-FB. Predicted occult movers may have their ITVs extended, or be selected for more resource-intensive adaptive strategies.