Patterns of recurrence in breast cancer patients after nipple-sparing and skin-sparing mastectomy
Leticia Alvarado Alvarado,
Guatemala
PD-0236
Abstract
Patterns of recurrence in breast cancer patients after nipple-sparing and skin-sparing mastectomy
Authors: Leticia Alvarado1, Dima Mahmoud1, Rejane Franco1, Philip Poortmans2, Orit Kaidar-Person3, Tarek Hijal1
1McGill University Health Centre, Division of Radiation Oncology, Montreal, Canada; 2Iridium Kankernetwerk, Division of Radiation Oncology, Wilrijk-Antwerp, Belgium; 3Chaim Sheba Medical Center, Breast Radiation Unit, Tel-Hashomer, Israel
Show Affiliations
Hide Affiliations
Purpose or Objective
Reports of residual breast tissue after nipple-sparing (NSM), and skin-sparing mastectomy (SSM), have raised concerns regarding safety as well as interest in determining patterns of recurrence in patients undergoing these trending surgical techniques, to better tailor systemic and local treatments.
Material and Methods
Data obtained from medical records of breast cancer (BC) patients, who underwent NSM and SSM at a single institution, between 2004 and 2018, were retrospectively analyzed to identify patients’ patterns of first breast cancer recurrence as well as their demographics, disease characteristics, systemic and surgical treatments, and the use of postmastectomy radiotherapy (PMRT)
Results
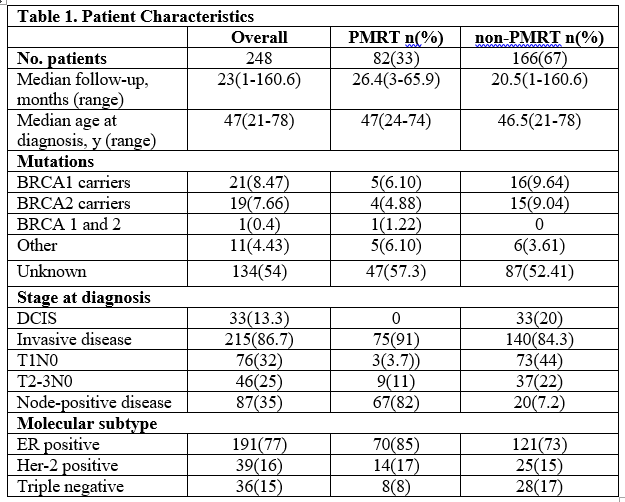
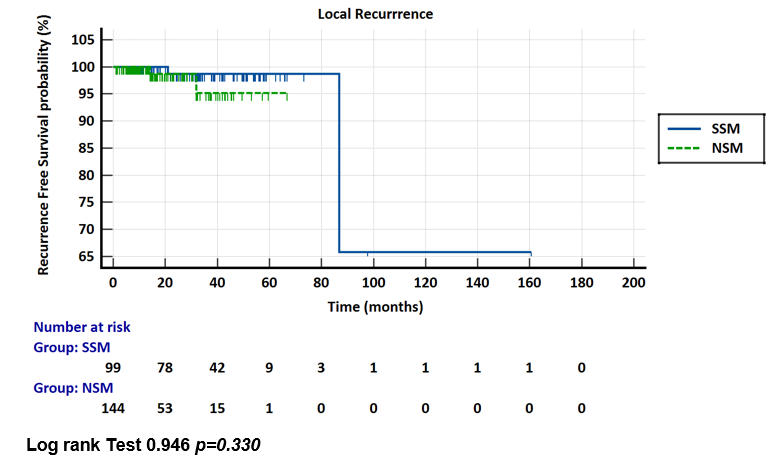
248 BC patients were identified, with a median age at diagnosis of 47-years(21-78), invasive disease in 215(86.7%) and DCIS in 33(13.3%). 144(58%) underwent NSM, and 104(42%) SSM. Overall, 33% received PMRT, 9(15%) patients with N0 disease, see Table 1 for detail. BRCA 1/2 mutations were identified in 41(17%) patients, although mutation status was not established in 54% of patients. 32% received preoperative chemotherapy while 35% did postoperatively. Of all first recurrences, 21%(4) were local, at scar level and 21%(4) were regional, at lymph node level; 58%(13) were reported as distant. No simultaneous loco-regional recurrence was reported, as well as no simultaneous loco-regional + distant recurrence. In terms of surgical technique, no significant difference was found regarding locoregional and distant recurrence when comparing NSM and SSM. In contrast, while comparing PMRT vs non-PMRT, more recurrence events, any kind (12 vs 9, p=0.04) and more distant recurrences (8 vs 5 p=0.009) were reported in the PMRT group. 98% of patients were alive at the time of last follow-up
Conclusion
A low rate of recurrence was observed in this large series of patients, operated for DCIS or invasive breast cancer with NSM or SSM, with no apparent difference in patterns of recurrence according to surgical technique. More local and distant recurrences were observed after PMRT, due to more advanced stage of disease allocated to this group. Further follow-up will allow to better define the long-term oncologic outcomes of these two techniques