Combining patient and population rectal shapes for re-irradiation of recurring prostate cancer
PD-0165
Abstract
Combining patient and population rectal shapes for re-irradiation of recurring prostate cancer
Authors: Sara Pilskog1,2, Andreas Størksen Stordal3, Liv Bolstad Hysing1,4, Christian Ekanger1, Øyvind Lunde Rørtveit1,4
1Haukeland University Hospital, Department of oncology and medical physics, Bergen, Norway; 2University of Bergen, Faculty of Mathematics and Natural Sciences, Bergen, Norway; 3NORCE Norwegian research centre, Department of Energy, Bergen, Norway; 4University of Bergen, Department of oncology and medical physics, Bergen, Norway
Show Affiliations
Hide Affiliations
Purpose or Objective
Balancing risk of toxicity against effect is challenging in re-irradiation of local recurrent prostate cancer, as dose-response data for these patients are non-existing. A pragmatic solution in order to avoid toxicity in our clinic is to crop the target volume to the rectal shape of the planCT, and thereby constraining target dose. Knowing that rectal motion varies among patients and that rectal shape changes can affect our decision, the objective was to develop a model that combines patient-specific rectal shapes with population motion patterns to assess the consequence of changes.
Material and Methods
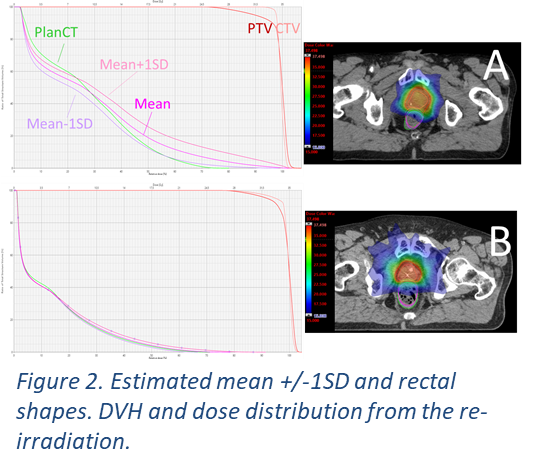
A Bayesian deformation model was used to combine the two patient-specific rectal shapes with the shape changes obtained from a population (Figure 1). The patient-specific rectal shapes in this case were shapes from the primary and the re-irradiation planCT, respectively (Figure 1, right). These patients belong to a cohort 39 patients treated for recurring prostate cancer. The rectum shapes from the two planCTs were deformably co-registered. Thereafter, the rectum shape of the second planCT was deformably registered to a population rectal shape (PRS). The PRS was obtained from >300 CTs in another cohort of 37 prostate cancer patients. The resulting deformation fields allow for analysis of probable motion patterns (Figure 1, left) and generation of new probable rectum shapes. The estimated shape of the mean rectum in the re-irradiation patients was found by shrinkage estimation, weighting the two patient-specific rectum shapes with the PRS. To estimate variations around this estimated mean shape, the Bayesian deformation model was used to interpolate probable deformation patterns that move the rectum into and out of the high dose volume. The mean rectum shape was deformed in this way by +/-1SD . To evaluate the impact of the changes we compared DVHs for the modelled mean rectum shape +/-1SD to the rectum shape in the planCT used for re-irradiation. 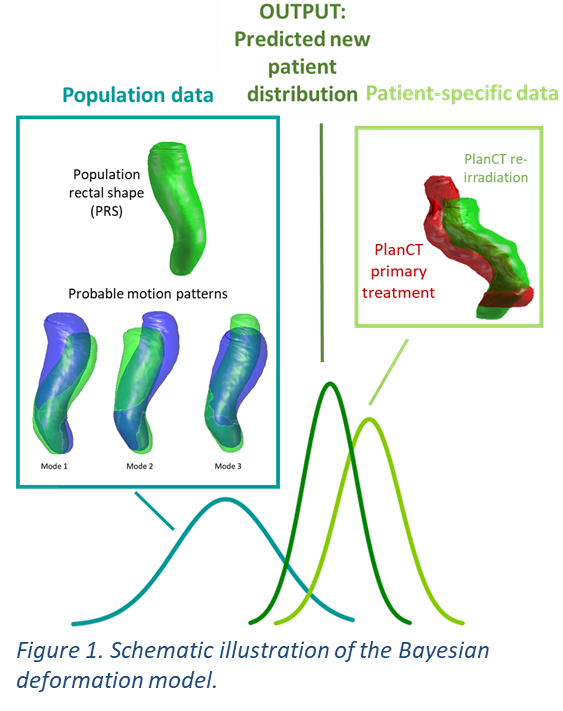
Results
The mean rectum shape was found by weighing the re-irradiation rectum shape by 50%, whereas the shape in the primary planCT and the PRS both were given 25% weight. Reason for reducing the weight of the older CT was that primary RT occurred in the years 2001-2010, thereby susceptible to alterations in preparation protocol. In Figure 2, the results for a patient (A) with small rectum for re-irradiation, a decrease of 30% as compared to the primary planCT and a patient (B) with larger rectum but no volumetric change compared to the primary planCT. Compared to the dose from the estimated mean+/-1SD, the rectal shape at planCT lead to an underestimation for patient A, whereas for patient B the dose to the estimated rectum shapes and the planCT was almost identical.
Conclusion
We presented a novel method combining patient-specific and population rectal shapes for use in decision-making of re-irradiation for prostate cancer. The model adjust to the variation of the two patient-specific inputs, and should be evaluated for more patients.