Tumor control after MR-guided adaptive stereotactic radiotherapy for adrenal metastases
Famke L. Schneiders,
The Netherlands
PD-0068
Abstract
Tumor control after MR-guided adaptive stereotactic radiotherapy for adrenal metastases
Authors: famke schneiders1, Claire van Vliet1, Miguel A Palacios1, Ben J Slotman1, Frank J Lagerwaard1, Anna ME Bruynzeel1, Suresh Senan1
1Amsterdam UMC, Radiation Oncology, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
SABR delivery to adrenal tumors can achieve high local control rates, with pooled analyses suggesting that a BED10 ≧70Gy is necessary. We implemented Stereotactic Magnetic Resonance Adaptive Radiotherapy (SMART) delivery using 3mm PTV margins and preferential avoidance of organs at risk (OARs). To evaluate the influence of target coverage compromise, we analyzed outcomes in 105 consecutive adrenal metastases treated using SMART at a single institution.
Material and Methods
Adrenal SMART was performed using (i) a 3D MR simulation during inspiration breath-hold for pretreatment delineation and generation of a treatment plan, (ii) daily 3D MR scan acquisition prior to each fraction, (iii) deformation and adjustment of OAR contours within 2cm of PTV on daily MR, and (iv) daily online plan reoptimization. The PTV was derived by adding a 3mm margin to the breath-hold GTV, and an ‘optimized’ PTV generated by excluding OARs. Online plan reoptimization aims to avoid high OAR doses. A step and shoot IMRT technique delivered in 1-8 fractions, with beam-on gating only when the target is inside the PTV margin. Visual feedback was provided to patients by an MR-compatible monitor projecting real-time 2D cine MR images. This retrospective study was granted exemption by our Medical Ethics Review Committee.
Results
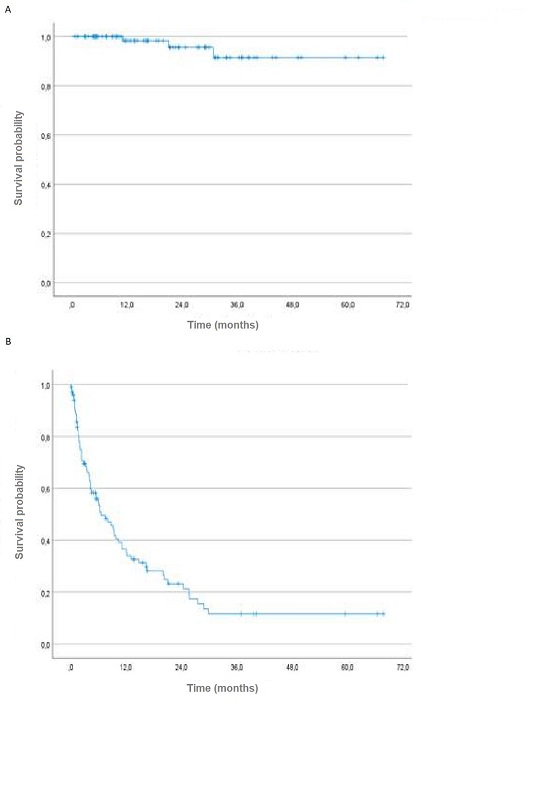
Between 2016-2022, SMART was performed in 105 adrenal metastases. Main primary tumors were lung (72%) and renal cancer (8%). Most schemes (90,5%) delivered a BED10 ≧70Gy. Delivery in <5 fractions was performed in 19%, and single fraction delivery (16-24Gy) in 10% of all patients (Figure 1). Maximum dose was 125-140% of prescribed dose. Using a D99 BED10 of <70 Gy, coverage of the ‘optimized’ PTV was compromised in 47% of patients due to OAR sparing. Planned fractions were completed in 97% of cases. Acute toxicity was maximum grade 2 in 61% of patients, one patient had grade 3 nausea. At a median follow up of 13 months (range 0-68 months), best local responses according to RECIST criteria were SD (33%), PR (42%) and a CR (22%). Local progression was observed in 3% of cases, and 78% had out-of-field progression (Figure 2). The 1-yr and 2-yr PFS rates were 37% and 24%, respectively, with a median time to progression of 7.5 months. The PFS did not correlate with dose. 52% of all patients underwent systemic therapy within 3 months of SMART, with 19% undergoing systemic therapy during SMART.
Conclusion
Despite preferential avoidance of OARs that led to compromised dose coverage in 47% of treated patients, adrenal SMART achieved high in-field tumor control. As 52% of all patients underwent systemic therapy within 3 months of SMART, our findings suggest that preferential OAR sparing to minimize risk of toxicity is acceptable in this patient population.
Figure 1. SMART dose fractionation schemes used for adrenal metastases at our institution.
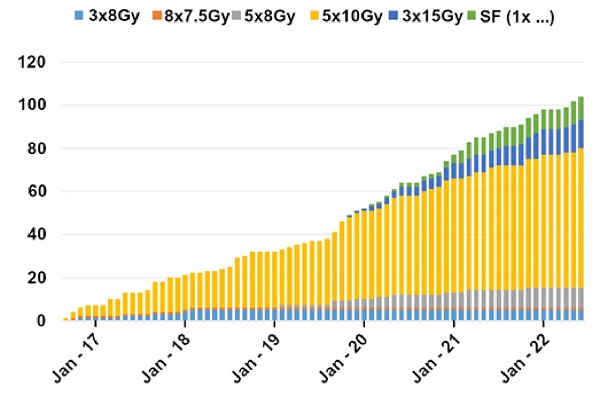
Figure 2. Kaplan-Meier curve of (A) Local Progression Free Survival (LPFS) and (B) Distant Free Survival (DFS)