Stereotactic ablative radiosurgery (SABR) for spinal metastases: 12-years of experience
M. Carmen Rubio Rodríguez,
Spain
PD-0655
Abstract
Stereotactic ablative radiosurgery (SABR) for spinal metastases: 12-years of experience
Authors: Raquel Ciervide1, Ovidio Hernando1, Mercedes López1, Ángel Montero1, Emilio Sánchez1, Beatriz Álvarez1, Mariola García-Aranda1, Jeannette Valero1, Xin Chen1, Karla Rossi1, Carmen Cañadillas1, Carmen Rubio1
1HM Hospitales, Radiation Oncology, Madrid, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Objective: To assess the clinical outcomes of patients with spine metastases treated with SABR at our institution.
Material and Methods
Material/Methods: Patients with spine metastases treated with SABR (1fraction/18Gy or 5fractions/7Gy) during the last 12 years have been analyzed. All patients were simulated supine in a custom cradle or with a shoulder mask depending on the spine location. 1mm slices CT images and MRI fusion were performed. Contouring was based on International Spine Radiosurgery Consortium Consensus Guidelines including the involved vertebral body, both pedicles and the grossly visible-tumor in the CTV. PTV margins were 0 (single dose) and 1mm (5 fractions). High conformal techniques (IMRT/VMAT) were used for treatment planning to accomplish coverage and international OAR constraints. Intra (X-Ray Exactrac) and interfraction (CBCT or X-Ray Exactrac) verification were mandatory.
Results
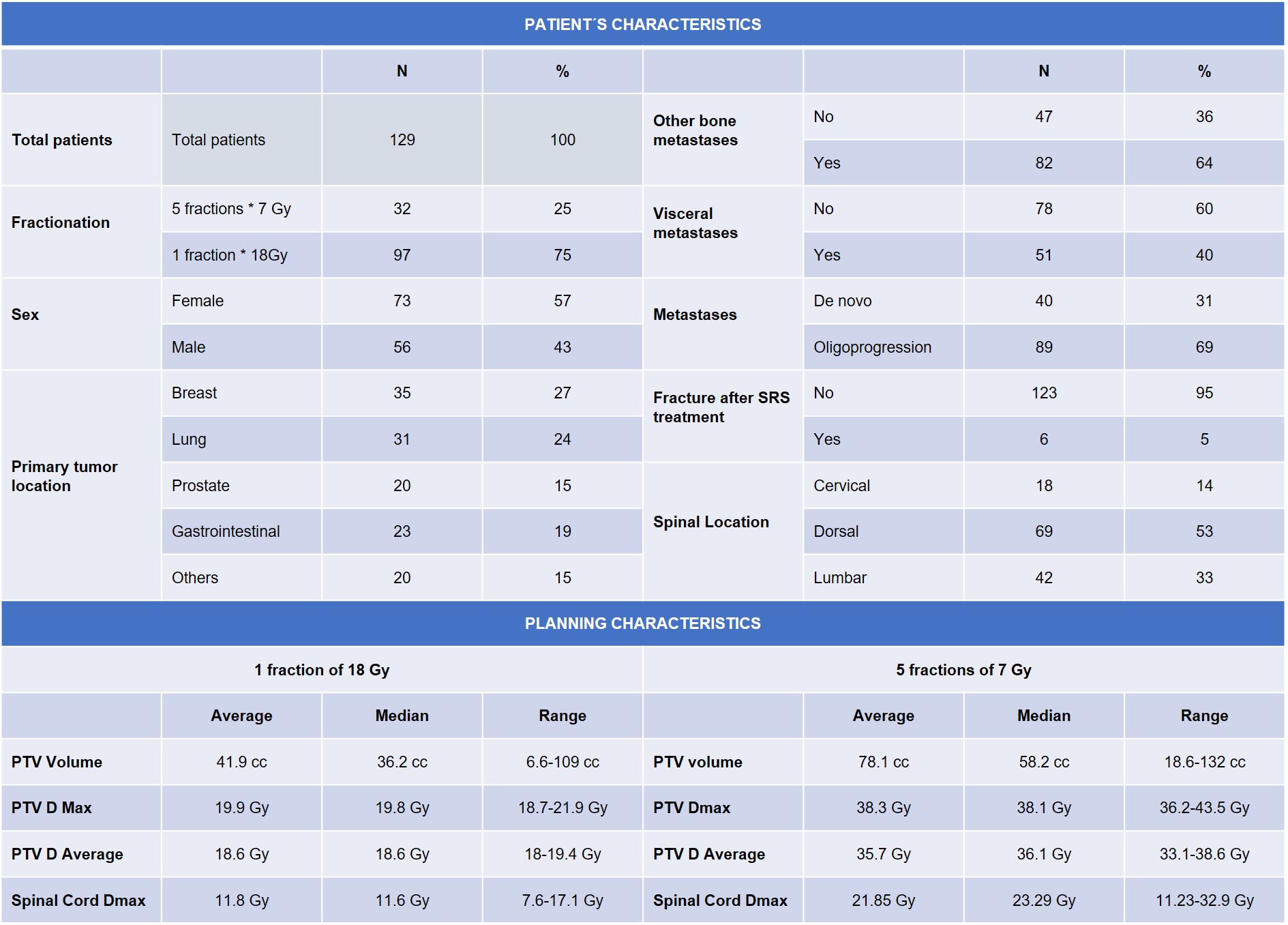
Results: From February 2010 to January 2022,129 patients with spinal metastases were treated with SABR. Patients‘ median age was 66years old(range 28-84). Patients’ and treatment planning characteristics´ are described in table1.
For patients with painful metastases (74/129:57%),100% experienced an improvement in pain after SABR which a median reduction of 4points (range1-8) in the Visual Analogue Scale (VAS).
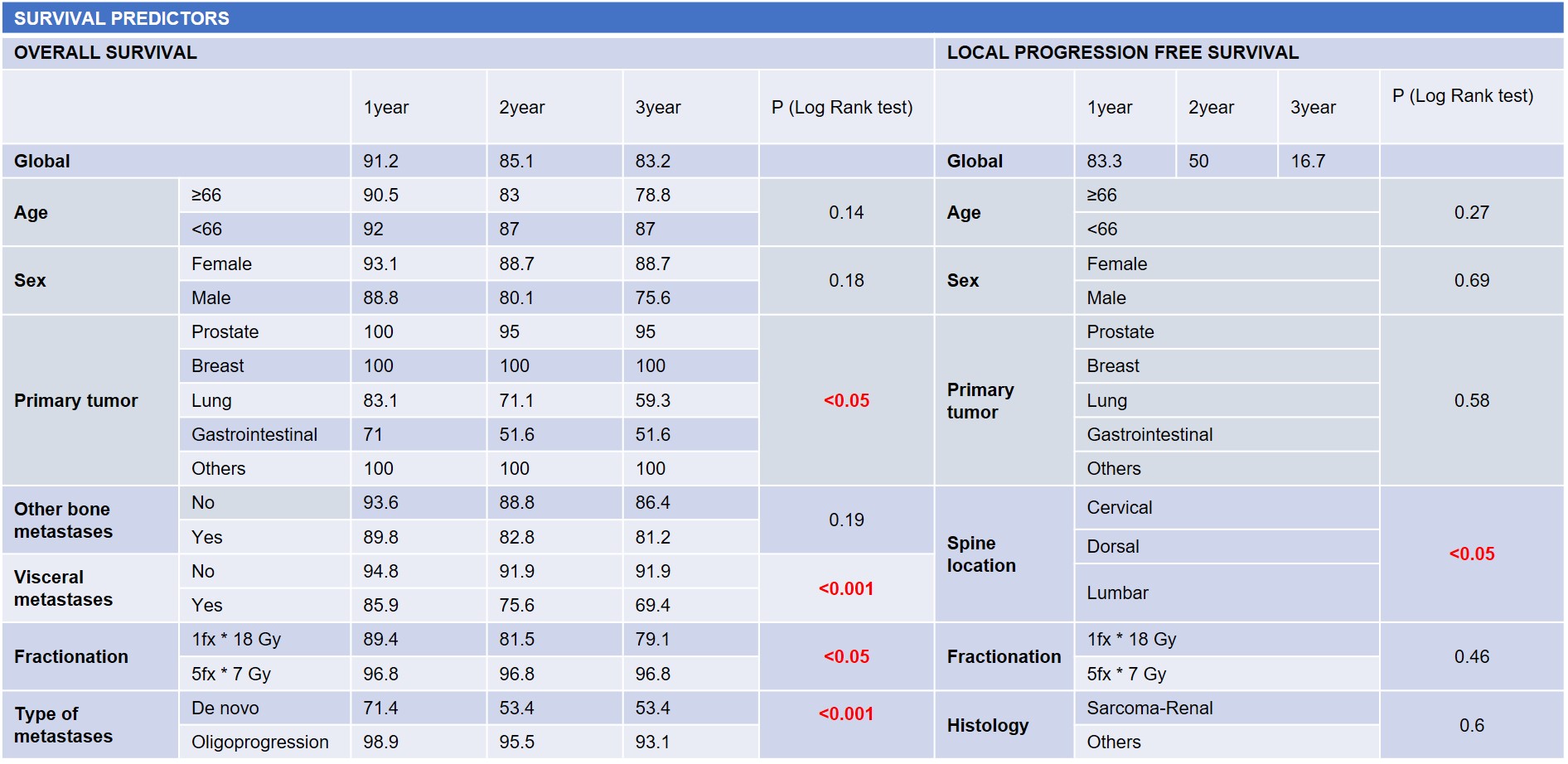
With a median follow up of 14.2 months (average 22.9; range 0.5-140) 6 patients (4.6%) experienced local relapse(1prostate, 1breast,1lung,1sarcoma and 2renal cancer). Local progression free survival was different considering metastasis’s location(p <0.04). The 1,2 and 3 years overall survival was 91.2, 85.1 and 83.2% respectively. Overall survival was significantly different according to primary tumor location (p<0.05) and worse when visceral metastases were present (p<0.05), if patients were metastatic de novo (p<0.05) and if 1fraction was delivered (p:0.01). We didn’t find any differences regarding histology, age, sex or if more bone metastases were present. Survival predictors are described in table2.
Conclusion
Conclusions: According to our experience, SABR for patients with spinal metastases was useful to improve pain control. Regarding different survival outcomes, an adequate selection of patients and radiation dose is essential to propose this ablative approach.