The CMOS detector was first exposed to a series of monoenergetic QA beam deliveries with varying energy, spot separation, and Monitor Units (MU) per spot.
The CMOS detector was able to measure clinical beams up to approximately 180 MeV without saturation.
In 70 and 150 MeV beams, the CMOS detector was able to measure in two dimensions without saturation, allowing spot separation to be tested and verified (Figure 1).
Current dead time between consecutive frames of 14 ms results in approximately 30% of spot positions missed at 50 MU/spot, increasing to 80% of spot positions missed at 10 MU/spot.
To identify treatment delivery error monitoring potential, the CMOS detector to identify treatment delivery errors, a QA plan (150 MeV, 50 MU/spot, 2.5 mm spot separation, 10×10 cm² field) was manually edited by the clinical staff to distort one spot position by 1.0 mm in one axis.
Information about the location and direction of this spot was intentionally withheld from the team conducting the CMOS analysis.
The misaligned beam can be identified as the antepenultimate spot in the x-axis.
Due to the position of the CMOS detector in the nozzle, the measured distortion was 0.77±0.01 mm.
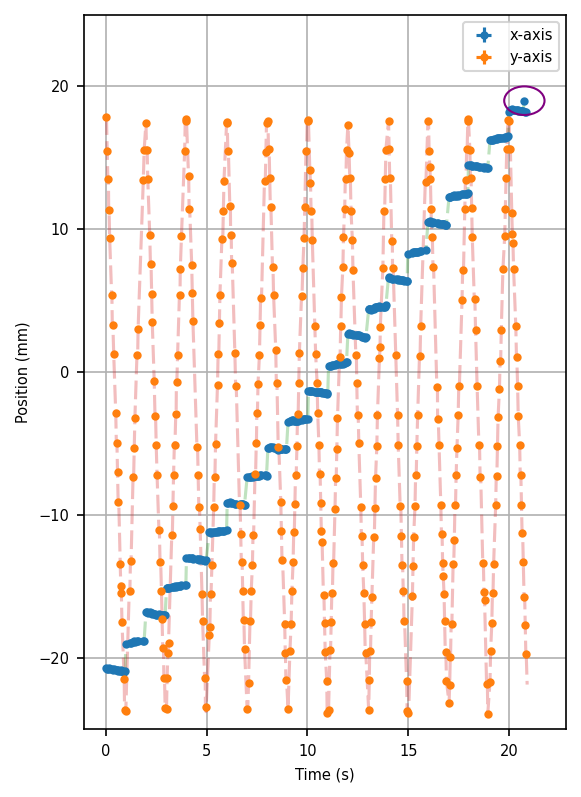
Figure 1: Measured beam positions by the CMOS detector, highlighting the intentionally misdelivered spot.
The CMOS detector was then irradiated with two clinical style fields to assess clinical practicability.
A comparison of the first energy layer between the TPS dose map and the CMOS detector can be seen in Figure 2.
Due to current dead time limitations, a thorough qualitative gamma comparison is not possible owing to missed spots, however many of the key features of the clinical plan (local hot-spots, overall shape) are visible in the CMOS measurement.
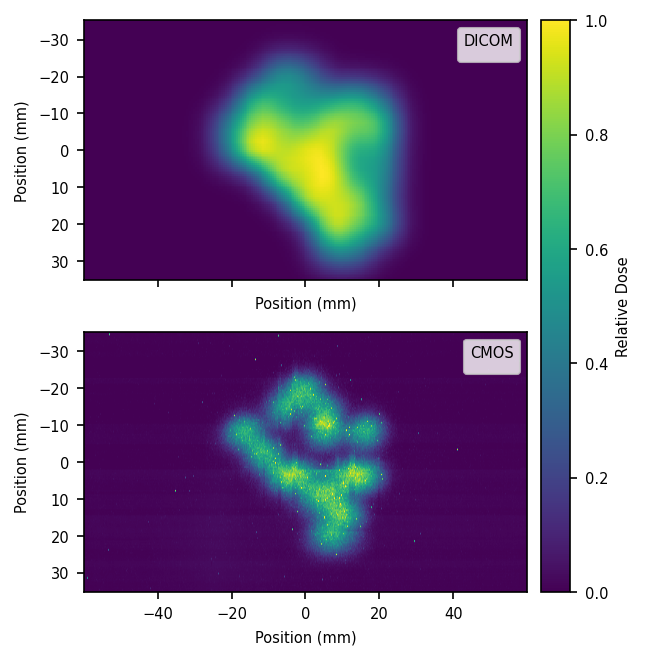
Figure 2: Comparison of measured (CMOS) and expected (TPS) dose distribution.