Exvivo proton range uncertainty verification of dose calculation on CTand CBCT based synthetic ct
JUAN MARIA PEREZ MORENO,
Spain
PO-1987
Abstract
Exvivo proton range uncertainty verification of dose calculation on CTand CBCT based synthetic ct
Authors: JUAN MARIA PEREZ MORENO1, Isabel Lorenzo Villanueva1, Rasmus Nilsson2, Sebastian Andersson2, Juan Antonio Vera Sánchez1, Juan Castro Novais1, Fernando Cerrón Campoo1, Elisabet Canals de las Casas1, Martin Janson2, Erik Engwall2, Alejandro Mazal1
1Quirónsalud Protontherapy Center, Radiation Oncology, Pozuelo de Alarcón (Madrid), Spain; 2RaySearch Laboratories, Research and Development, Stockholm, Sweden
Show Affiliations
Hide Affiliations
Purpose or Objective
To estimate dose calculation range uncertainty in CT images and synthetic CT from CBCT of an in-house exvivo phantom.
Material and Methods
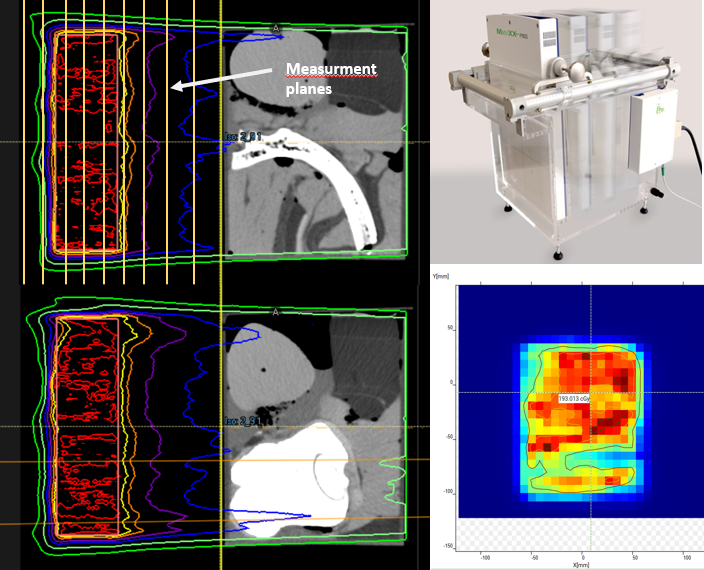
Using pork and cow exvivo tissues an in house phantom has been built. A single beam PBS plan has been optimized in Raystation 11B in with the aim to achieve a uniform dose distribution with a constant physical range in water behind the ex-vivo phantom (Fig 1).
The resulting PBS plan was recalculated on a synthetic CT based on a CBCT acquired in a Proteus One proton system. The synthetic CT was generated using the “Virtual CT” (VCT) algorithm of RayStation 12B, that includes a method for deforming the planning CT to the CBCT geometry combined with corrections for large differences in air/lung regions between the planning CT and the CBCT
Using a 2D array of parallel plane ion chambers MatriXX One in a DigiPhant PT water phantom with a housing for the detector, a series of planes at different depths were measured. A 3D dose distribution is reconstructed by stacking the planes measured.
Depth dose profiles were extracted from the MatriXX stacked measurement and from the TPS 3D dose distribution respectively, matching coordinates of every MatriXX detector in regions with doses over 80% of maximum dose at center of SOBP. For every depth dose line R90, R80 and R50 were extracted.
Results
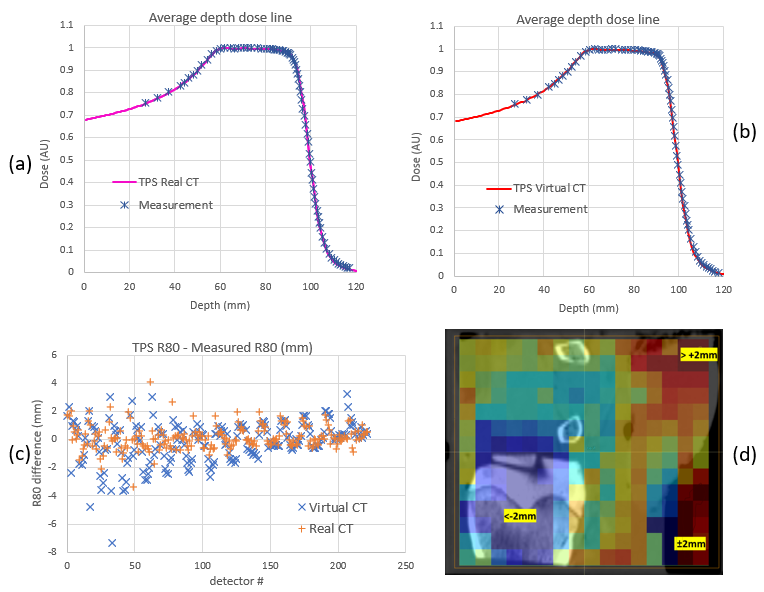
223 dose lines have been evaluated. Figure 2a and 2b show the average over all detectors of measured depth dose line versus average lines calculated in TPS for CT and VCT.
In Figure 2c the difference between measurement and calculation of R80 parameter for every detector is shown. Figure 2d shows a heat map of error ranges in VCT calculation with errors larger than 2mm in dark blue (underestimation) and dark red (overestimation). They are located in air-tissues interfaces and in high density bone areas.
For calculation on real CT, average of R90, R80 and R50 TPS-MatriXX differences is 0.11 mm and standard deviation (SD) of 0.89 mm. Assuming uncertainties of 0.2mm in R-values evaluation, 0.3mm in patient setup and k-factor of 2, would yield an estimated uncertainty in range calculation of about 1.6%, normalizing at 10 cm of physical phantom thickness
For VCT calculation, mean range error is -0.19 mm and SD of 1.51 mm with an estimated range uncertainty of 2.9%.
Conclusion
Described procedure yields an estimated range calculation uncertainty of 1.6% for the chosen tissue configuration in a real CT. In VCT the estimated uncertainty increases up to 2.9%, a value that could be used for on-line adaptive proton therapy workflows.
These uncertainties could be reduced excluding from analysis areas of high uncertainty due to air-tissue interfaces. 2.9% could be low enough to assess actual dose delivery with less uncertainty than QA CTs, as the image is acquired in treatment position. The validation of this results with different setups and/or tissues configuration could yield to an actual department range uncertainty estimation and help to reduce range margin in robust treatment planning.