Knowledge-based planning for intensity-modulated proton therapy of the brain and base-of-skull
PO-1968
Abstract
Knowledge-based planning for intensity-modulated proton therapy of the brain and base-of-skull
Authors: Robert Kaderka1, Nhan Vu1, Michael Butkus1
1University of Miami, Radiation Oncology, Miami, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Knowledge-based planning (KBP) automates treatment planning with a focus on efficiency, quality and reducing plan variability. We developed and evaluated a KBP model for brain and base-of-skull (BOS) targets treated with intensity-modulated proton therapy (IMPT).
Material and Methods
Commercial software was used to build a KBP model that creates dose predictions and optimization objectives. The model was trained with 89 patient plans treated at our institution, all optimized to a CTV employing robust optimization. In the training set, n=78 received 46-60Gy and n=11 were re-treats prescribed ≤35Gy.
While KBP predicts dose distributions, previous literature shows that fine-tuning optimization objectives and priorities in the model can substantially increase resulting plan quality. 20 patients were chosen for re-planning and subsequent iterative adjustment of optimization parameters.
The final model was then tested by re-planning an independent set of 27 patients that were not included in training. Plan quality was evaluated by comparing dosimetric parameters of body, CTV, brainstem, cochlea, eye, hippocampus, lens, optic chiasm/nerves, pituitary and skin of the KBP plans to the manual clinical reference. Paired t-tests tested for significance (p<0.05).
Results
The KBP model was finalized after two iterations to objectives and priorities. This model created clinically acceptable plans for all 27 test plans. The only significant differences between the manual and the KBP plans were CTV D0.03cc (mean manual: 108.4%, mean KBP: 110.0%, p=0.001), CTV Dmin (84.6%/80.4%/p=0.009), and pituitary gland D0.03cc (2181cGy/1792cGy/p=0.021). No other parameters were significant. CTV D0.03cc, DMin and V100% parameters for all patient plans are shown in Fig. 1. The x-value of each point represents the manual plan value and the y-value the KBP plan. It visualizes the lower CTV min doses and higher hot spots for KBP plans but indicates the same overall target coverage as measured by the V100% parameter.
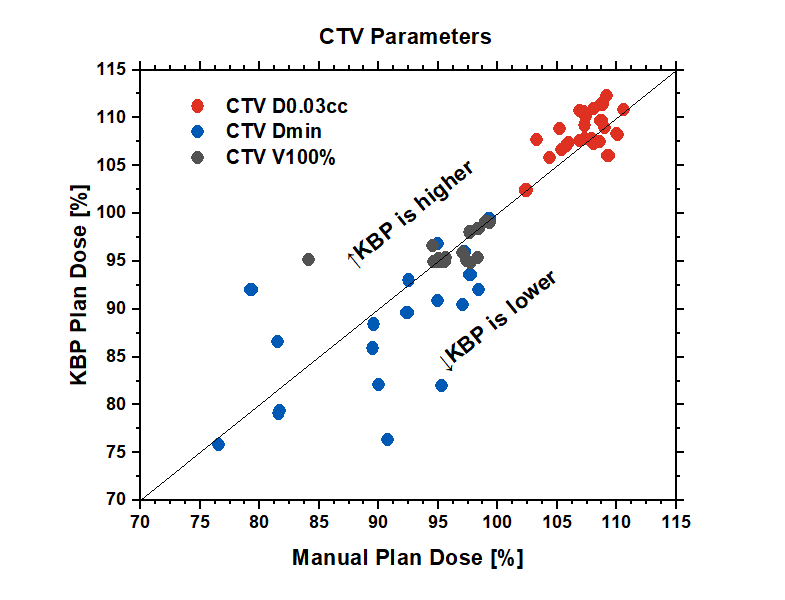
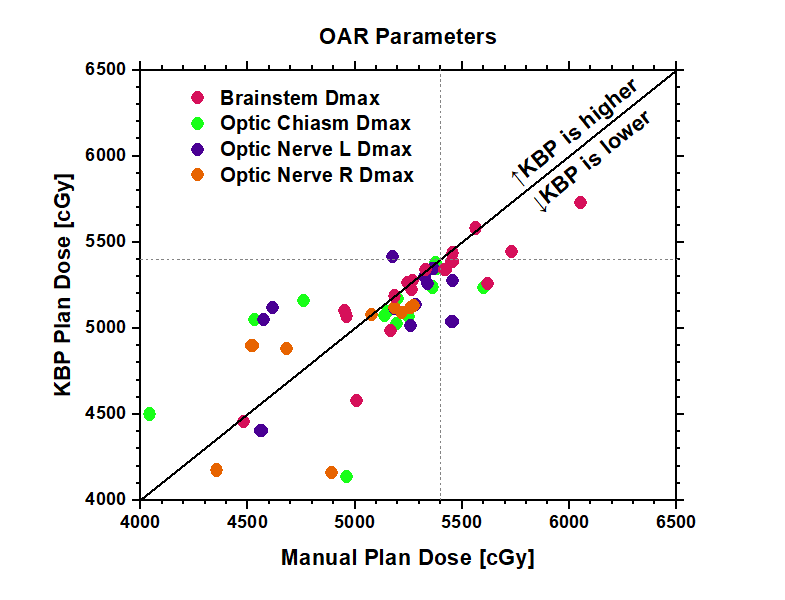
Fig. 2 illustrates the high dose area for the brainstem, optic chiasm and optic nerves. While the difference to the manual plans is not significant, we observe a trend where (by design) the KBP model strongly tries to push the max dose to these organs below 54Gy while the manual planner allowed higher doses in some cases. This could potentially explain the lower min point doses observed in the KBP plans.
Conclusion
A KBP model was developed and demonstrated to produce clinically viable plans for brain and BOS IMPT. In some cases lower min doses and higher hot spots are observed, but target coverage is comparable. The KBP model was built to strongly push for sparing of critical OARs. As with all plans intended to treat patients, KBP plans need careful evaluation and may require manual adjustment in order to achieve the desired compromise of target coverage and OAR sparing. Following the results of the evaluation, the model has been employed clinically.