Isotoxic dose escalation with proton beam therapy for distal oesophageal cancer
Mme Esien,
United Kingdom
PO-1966
Abstract
Isotoxic dose escalation with proton beam therapy for distal oesophageal cancer
Authors: Mme Esien1, Ahmed Abbas2, Christopher Rose3, Sarah Gwynne4, Owen Nicholas4, Richard Hugtenburg2,3
1Swansea University, School of Medicine , Swansea, United Kingdom; 2Swansea University, School of Medicine, Swansea, United Kingdom; 3Swansea Bay University Health Board, Medical Physics and Clinical Engineering, Swansea, United Kingdom; 4South West Wales Cancer Centre, Oncology, Swansea, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Dose escalation in oesophageal cancer (OEC) has potential to improve TCP and overall survival, but so far clinical trials have been negative, possibly due to increased dose to critical OARs. SCOPE 2, a current photon RCT limits dose escalation of GTV to 60Gy. Proton beam therapy (PBT) offers the possibility of dose escalation to GTV with same or reduced dose to OAR because of its physical properties. This work investigates the feasibility of Isotoxic dose escalation of GTV to 70Gy using PBT for distal OEC.
Material and Methods
Proton treatment plans were created using Eclipse™ v13.7 TPS from on anonymised patient 4DCT scans obtained from RTQA database (NeoScope). Isotoxic dose escalation from nominal plan of 50Gy to 55Gy, 60Gy, 65Gy and 70Gy was done, while maintaining 50Gy to ITV. Multi-beam plans were robustly optimised and evaluated for 12 uncertainty scenarios using SCOPE 2 protocol OAR constraints. Results were reported for the second-worst scenario. All plans were deemed clinically acceptable by a clinical oncologist.
Results
Table 1: Dose escalation statistics showing a sample result for robustly optimised dose escalations at 55Gy, 60Gy, 65Gy, and 70Gy. The result is given for the second worst-case scenario. For each dose escalation scenario, the prescribed dose to ITV was maintained at 50Gy.
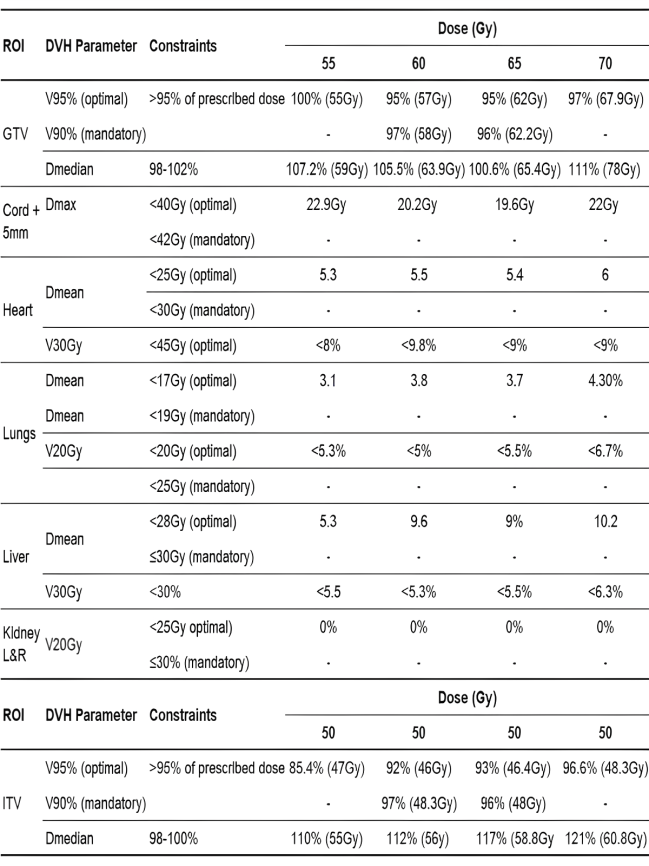
Escalating dose to GTV increased dose to OAR, but constraints were met with acceptable GTV coverage. Adding extra beams improved the dose distribution conformity to the GTV, limiting dose to OAR.
Conclusion
The results show that dose escalation to GTV to 70Gy may be achieved with a multi-beam configuration, without significant increased risk to OARs. Effective management of dose gradient between ITV and GTV is critical for successful dose escalation. Isotoxic dose escalation to GTV in distal OEC appears feasible with PBT, however further work is required in a larger sample, taking into consideration additional uncertainties such as motion and variable RBE.