Linear Energy Transfer Distributions for Pencil Beam Scanning of Pediatric Brain Tumors
Peter Laegdsmand,
Denmark
PO-1961
Abstract
Linear Energy Transfer Distributions for Pencil Beam Scanning of Pediatric Brain Tumors
Authors: Peter Laegdsmand1, Anne Vestergaard1, Ludvig Muren1, Yasmin Lassen-Ramshad1, Laura Toussaint1
1Aarhus University Hospital, Danish Center for Particle Therapy, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
The relative biological effectiveness (RBE) uncertainties associated with the variation in linear energy transfer (LET) of proton beams is a challenge for treatment planning of pediatric central nervous system (CNS) tumors near the brainstem. However, the LET distributions of pencil beam scanning (PBS) plans still need to be investigated for these patients. Therefore, our study aimed to survey the distribution of LET and RBE in the brainstem for patients treated at our institution.
Material and Methods
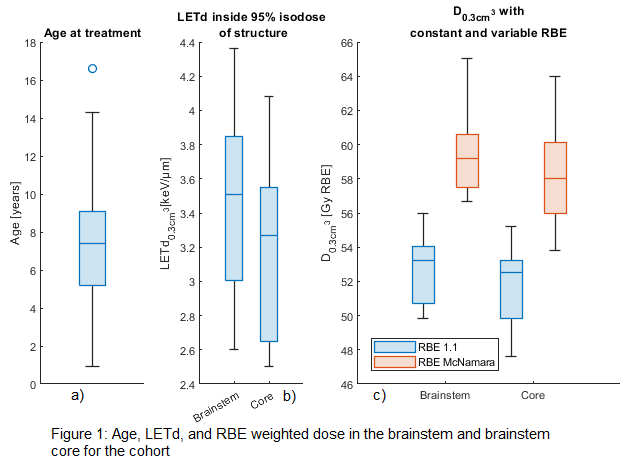
A cohort of 15 patients was selected from 47 pediatric CNS patients (aged less than 18 years (figure 1a)) treated with PBS. None had experienced brainstem toxicity. The selection criteria were: 1) Focal brain irradiation only, 2) Maximum dose to the brainstem at least 50 GyRBE. All plans used a minimum of 3 fields spaced by at least 30 degrees to mitigate high LET. The prescribed dose was 50.4 GyRBE (6 plans) or 54 GyRBE (9 plans) in 1.8 GyRBE fractions. Some plans included a boost of 5.4 GyRBE to a smaller target volume not considered in this study. The brainstem core was defined as the brainstem subtracted a 3 mm margin in the transversal directions. The dose-averaged LET (LETd), including only protons, was calculated for all plans by Monte Carlo simulations in Tool for Particle Simulation (TOPAS) v.3.5. Variable RBE was calculated for all plans on a voxel-level using the McNamara model with an 𝛼/𝛽 ratio of 2 Gy. D0.3cm³ in the brainstem and brainstem core was evaluated for a constant RBE of 1.1 and the McNamara RBE. LETd0.3cm³ was evaluated in the overlap between the 95% isodose and the brainstem/brainstem core.
Results
The maximum LETd in the brainstem varied considerably between plans. The interquartile range of LETd0.3cm³ at the 95 % cutoff was 0.8 keV/µm, the maximum was 4.4keV/µm (figure 2), and the median was 3.5 keV/µm (figure 1b). LETd0.3cm³ in the brainstem core tended to be slightly lower with a median of 3.3keV/µm. Taking variable RBE into account, D0.3cm³ increased from 53.2 GyRBE (RBE 1.1) to 59.2 GyRBE (McNamara RBE). Brainstem core median D0.3cm³ rose from 52.5 GyRBE (RBE 1.1) to 58 GyRBE (McNamara RBE). For five patients, brainstem D0.3cm³ was greater than 60 GyRBE with the McNamara RBE (figure 1c). All of these patients were below the age of six years at treatment. In two of them, the clinical target volume (CTV) was posterior to the brainstem, in two, the CTV was superolateral to the brainstem, and in one, the CTV wrapped around the brainstem. In all five patients, the CTV overlapped partly with the brainstem. Four of them had three-field plans, but one of them had five fields.

Conclusion
Even when field configurations are chosen to mitigate elevated LETd, there are still regions in the brainstem in some patients with relatively high LETd and dose. There is no significant clinical evidence that this increases the risk of brainstem toxicity. However, new strategies for reducing LETd in the brainstem and other high-risk organs for PBS should be investigated.