PBS proton arc therapy may improve focal boosting compared to VMAT for localised prostate SBRT
PO-1955
Abstract
PBS proton arc therapy may improve focal boosting compared to VMAT for localised prostate SBRT
Authors: Robin De Roover1,2, Cédric Draulans3, Kenneth Poels1,2, Erik Engwall4, Viktor Wase4, Otte Marthin4, Johan Sundström4, Sofie Isebaert1,2,3, Uulke van der Heide5, Tom Depuydt1,2,3, Karin Haustermans6,2,3
1University Hospitals Leuven, Department of Radiation Oncology, Leuven, Belgium; 2University Hospitals Leuven, Particle Therapy Interuniversity Center Leuven – PARTICLE, Leuven, Belgium; 3KU Leuven, Department of Oncology, Leuven, Belgium; 4RaySearch Laboratories, Research and Development, Stockholm, Sweden; 5The Netherlands Cancer Institute, Department of Radiation Oncology, Amsterdam, The Netherlands; 6University Hospitals Leuven, Department of Radiation Oncology, , Leuven, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
In the phase III FLAME trial a dose response relationship to the intraprostatic GTV D98% has been shown leading to improved biochemical disease-free survival for localised prostate cancer (PCa). In the current study, a novel treatment planning system prototype build for PBS proton arc therapy optimization is explored to investigate whether PBS proton arc therapy could improve focal dose escalation to the GTV while maintaining similar or reduced dose to the critical organs at risk (OAR) compared to contemporary photon VMAT.
Material and Methods
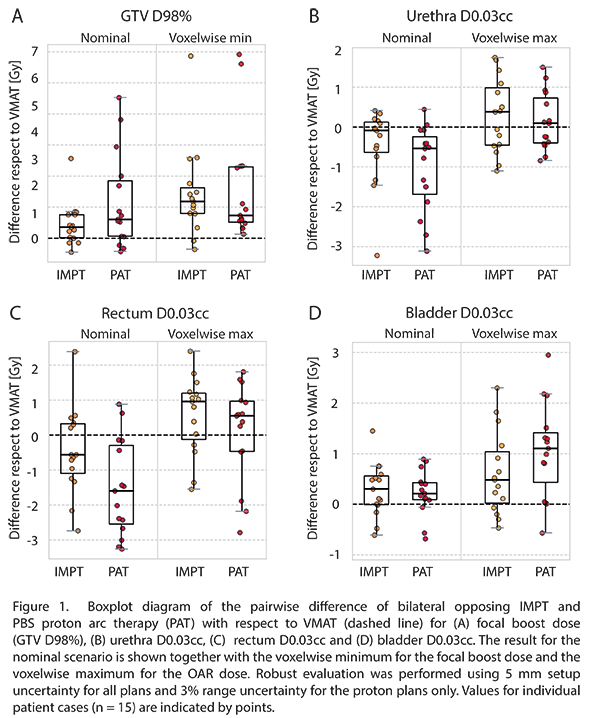
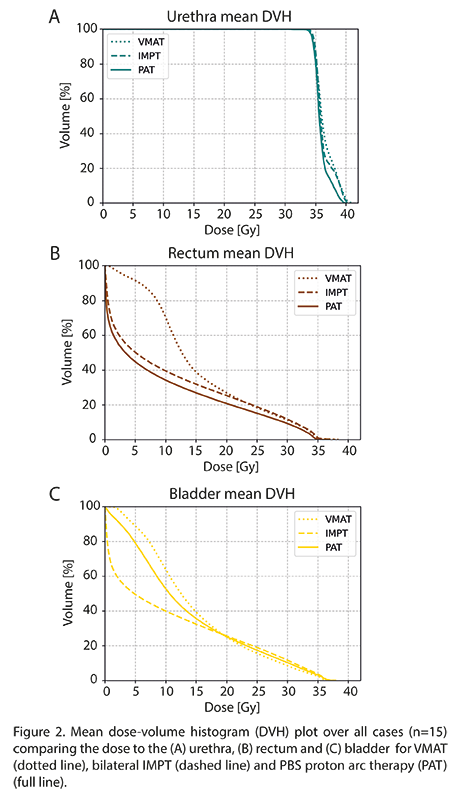
Fifteen men with localised PCa previously treated in the hypo-FLAME and hypo-FLAME 2.0 trials were replanned using VMAT, bilateral opposing IMPT and PBS proton arc therapy (PAT). The prescribed dose was 35 Gy to the prostate (CTVp1) and 30 Gy to the seminal vesicles (CTVp2) in 5 fractions. The focal boost was up to 50 Gy if the dose to the OAR permitted so. Both photon and proton plans were robustly optimized in a research version of RayStation 11B using 5 mm setup uncertainty. For proton plans 3% range uncertainty was included. VMAT plans were generated for 6MV FFF on a Varian TrueBeam STx and consisted of two full arcs with collimator angles 10° and 80°. Proton plans were generated for an IBA ProteusONE compact gantry. Bilateral opposing IMPT plans consisted of two beams at gantry angle 90° for couch angles 0° and 180°. PAT plans consisted of two partial arcs going from 100° to 325° gantry angle for couch angles 0° and 180°. The gantry angle spacing between two consecutive energy layers was set at 4° resulting in 34 energy layers per arc, each at a different gantry angle. The focal boost dose (GTV D98%), the target coverage (CTVp1 and CTVp2 D98%) and dose to the critical OAR (rectum, bladder and urethra) were compared for the nominal scenario. Robust evaluation (5mm-(3%)) was performed to compare the voxelwise minimum (VWmin) focal boost and target dose and the voxelwise maximum maximum dose (D0.03cc) to the critical OAR. Statistical testing comprised of a Friedman test followed by Wilcoxon signed-rank tests.
Results
PAT plans achieved higher GTV D98% in the nominal scenario compared to VMAT with a median difference of 0.7 Gy (p<0.01) and >3 Gy for 3/15 patients (Fig 1A). In addition, PAT plans had higher VWmin GTV D98% compared to VMAT. IMPT also showed improved GTV D98% over VMAT but had a smaller increase. All techniques had similar target coverage. Compared to VMAT, PAT plans had reduced D0.03cc in the nominal scenario to the urethra (Fig 1B), median -0.5 Gy (p<0.01), and rectum (Fig 1C), median -1.6 Gy (p<0.01), but showed increased D0.03cc to the bladder (Fig 1D), median 0.2 Gy (p=0.04). IMPT had no significant reduction in nominal D0.03cc to the urethra and rectum. The mean DVH for the critical OAR is shown in Fig 2.
Conclusion
PBS proton arc therapy has the potential to improve focal boosting to the intraprostatic GTV while reducing the dose to the urethra and rectum and could thereby enhance treatment outcome for selected PCa patients.