The synthetic CT for CBCT-based online adaptive radiotherapy: challenges and QA
PO-1728
Abstract
The synthetic CT for CBCT-based online adaptive radiotherapy: challenges and QA
Authors: Sonja Wegener1, Stefan Weick1, Robert Schindhelm1, Otto A. Sauer1, Joerg Tamihardja1, Gary Razinskas1
1University of Wuerzburg, Radiation Oncology, Wuerzburg, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
Ethos enables online-adaptive radiotherapy based on daily CBCT. Clinical treatment on Ethos began with the pelvic region (Sibolt et al. 2020), but investigations in an emulated environment suggest that treatments of the head-and-neck region are also feasible (Yoon et al. 2020). Density maps for dose calculation in adaptive treatments are based on a deformed registration of the planning CT (pCT) onto the CBCT, called synthetic CT (sCT). Incorrect sCTs can lead to dose calculation errors. Therefore, the sCTs for two regions with large density differences and geometrical changes were examined. Different means of quality assurance were evaluated.
Material and Methods
pCTs were acquired of a slab phantom covered with 5 mm bolus. 3D-printed spacer rings between the phantom surface and the bolus introduced air gaps of different s. Adaptive treatment plans were irradiated on Ethos combining different air gaps during pCT and CBCT. Densities in the sCTs were compared to regular CT images. Adaptive treatments were also performed for the neck region of an Alderson Rando phantom with standard and customized bolus to generate sCTs for evaluation.
For a CIRS Dynamic Thorax Phantom, pCT and CBCT with different spherical lung tumor inserts of 1 cm, 2 cm or 3 cm diameter were combined in adaptive treatments. Treatment plans were recalculated in Eclipse. Secondary dose was calculated using Mobius3D and RadCalc. EPID exit dosimetry was obtained using RadCalc. All calculations were either based on the CBCT or the sCT.
Results
The use of different air gaps during pCT and CBCT resulted in highly variable bolus thickness in the sCT with errors exceeding 5 mm. In extreme cases, air gaps were filled with the density of the surrounding material (Figure 1a) or the phantom was unrealistically deformed in the vicinity of the changed bolus geometry (Figure 1b). The same changes, i.e. increased bolus thickness (A) and deformation (B), were visible on an anthropomorphic phantom using standard bolus (Figure 2a). The use of customized bolus reduced the effects (Figure 2b).
Changes in lung inserts were not properly taken into account in the sCTs. This resulted in target mean dose calculation errors of up to -16% for the adaptive and 12% for the scheduled plan. Secondary dose calculation based on the same sCT, using Mobius 3D, showed acceptable agreement to the Ethos calculation, failing to detect the errors. However, EPID dosimetry and dose calculation on the CBCT yielded reduced Gamma passing rates and predicted changed target doses.
Conclusion
In several situations, sCTs did not yield the correct density distribution. Avoiding air gaps below bolus seems favorable for sCT generation, so the use of customized bolus should be further investigated. Additional quality assurance for the sCT, such as a secondary dose calculation based on the CBCT density or EPID in-vivo dosimetry, is recommended especially in anatomical regions with large density differences.
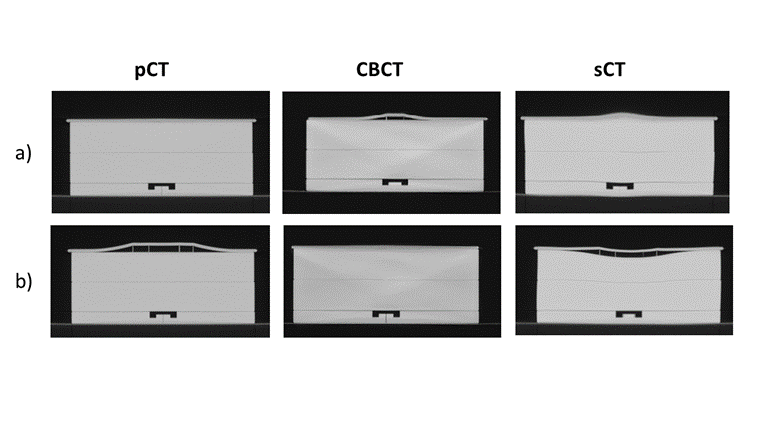
Figure 1
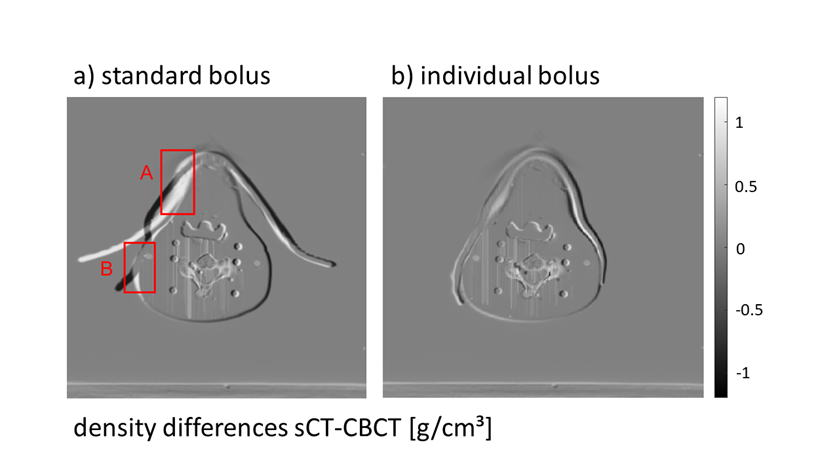
Figure 2