Increased clinical utility of MC secondary dose calculation vs state-of-the-art analytical algorithm
PO-1717
Abstract
Increased clinical utility of MC secondary dose calculation vs state-of-the-art analytical algorithm
Authors: Mai-Britt Linaa1, Ditte Sloth Møller1, Markus Alber2, Simon Nyberg Thomsen3, Lone Hoffmann1
1Aarhus University Hospital, Department of Oncology, Aarhus, Denmark; 2Heidelberg University Hospital, Department of Radiation Oncology, Heidelberg, Germany, Germany; 3Aarhus University, Dept. of Clinical Medicine, Faculty of Health Science, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Independent secondary dose calculation (ISDC) is becoming an essential element of patient-specific QA. Here, we explore the question whether the increased accuracy of a Monte-Carlo based system with customized beam models translates into a clinical benefit compared to a Convolution-Superposition algorithm with generic beam models.
Material and Methods
For a set of 95 consecutive patients grouped into 19 case classes, treatment plans were re-calculated with SciMoCa v1.5.2 (Radialogica, St. Louis, USA) and Mobius v3.1(Varian, Sunnyvale, USA) and subsequently analysed with various Gamma and DVH criteria. The treatment planning system was Eclipse v15.6 (Varian, Sunnyvale, USA) using the Acuros algorithm. In order to increase sensitivity of ISDC, the strictest criteria that still produced acceptable levels of false positives were identified. Failing treatment plans were analysed by various modulation complexity measures and for other sources of disagreement to the TPS.
Results
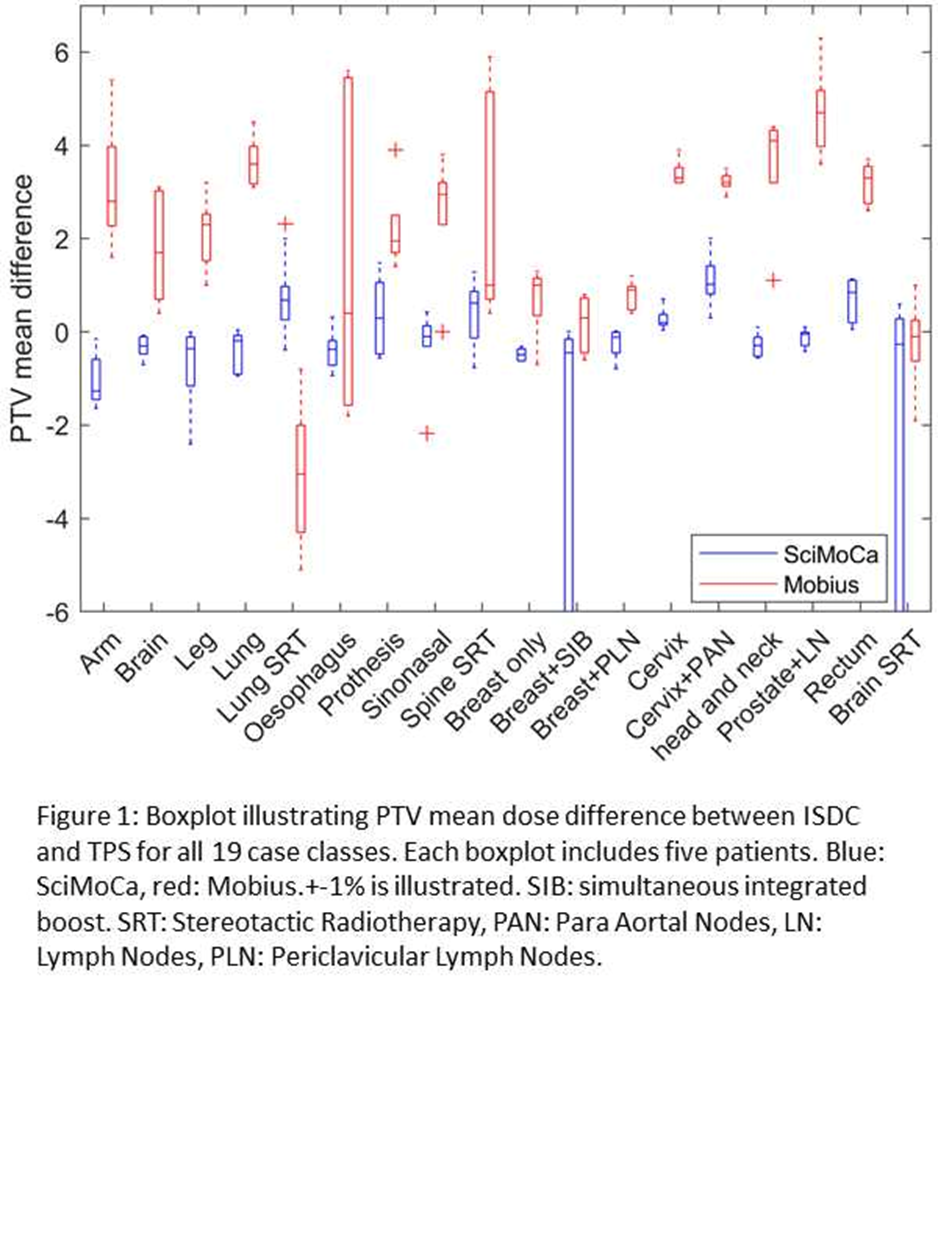
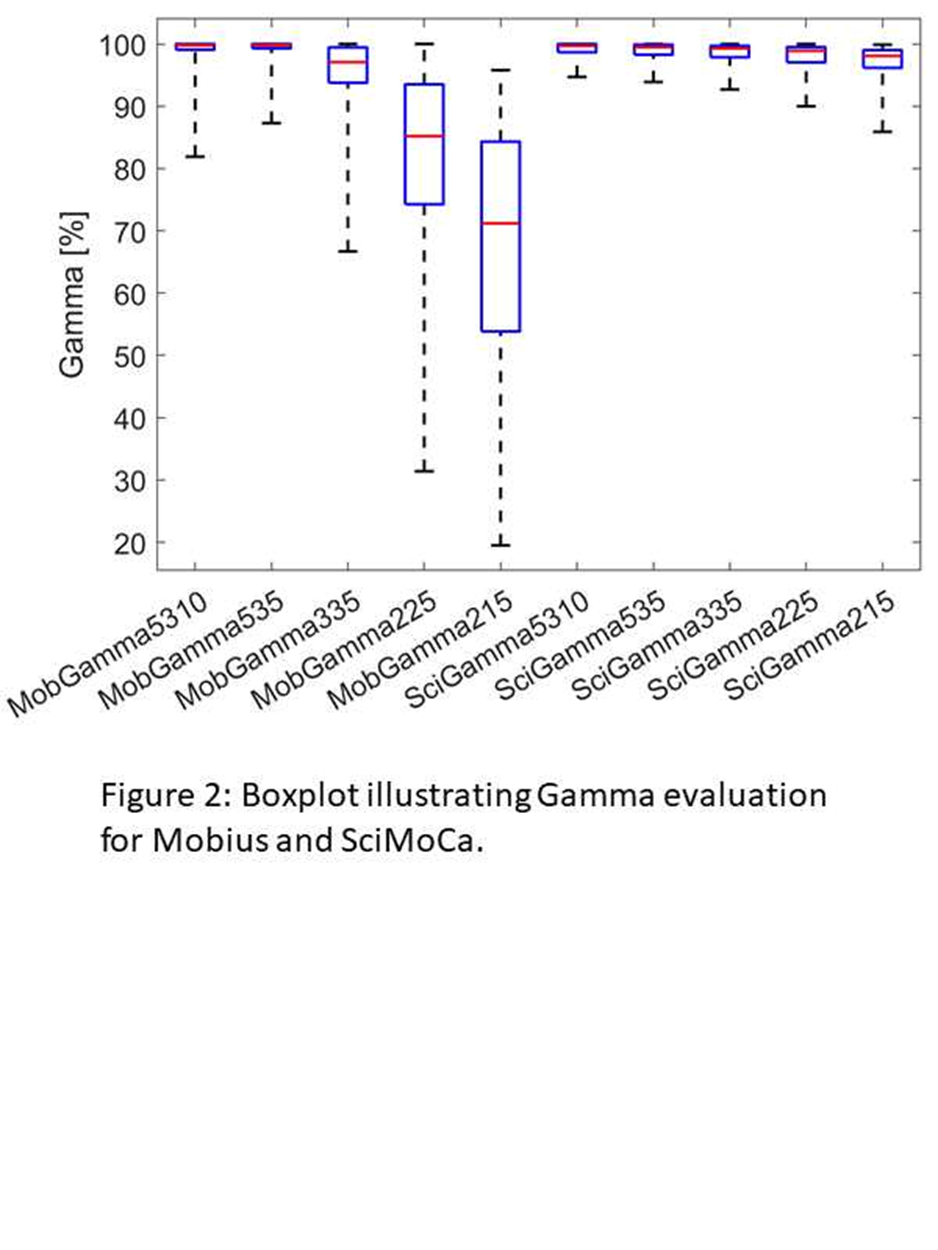
Agreement of mean PTV dose varied from -4% to 4% depending on case class for Mobius, see Fig 1. SciMoCa agreed with the TPS within +-2% for nine case classes and within +-1% for 17 case classes, except for 3 outliers. In the remaining two case classes, large deviations were seen for one patient in each class. For the breast case, the deviations were due to surgical clips in the target. For the stereotactic case being a brain tumor (Volume of GTV was 0.3ml), very small field s were used. Gamma 5%/3mm (the vendor recommendation for Mobius) resulted in pass rates > 85% across all case classes with the majority of patients > 95%. A similar result was found for SciMoCa for Gamma 2%/1mm. There was no correlation between modulation degree measures and outlier plans for SciMoCa, whereas Mobius struggled with high-modulation and stereotactic case classes. Investigation of SciMoCa outliers revealed differences in patient density definitions (bolus, immobilisation, air) and limitations of the TPS dose calculation. There was no pattern for Mobius outliers.
Conclusion
The higher consistency and accuracy of Monte-Carlo allows much stricter acceptance levels. Consequently, outliers could be traced back to planning and TPS issues that were worthy of investigation with high specificity. This result is likely also a consequence of customized beam models.