Cone beam CT-based dose recalculation as plan-specific QA in online adaptive radiotherapy
PO-1705
Abstract
Cone beam CT-based dose recalculation as plan-specific QA in online adaptive radiotherapy
Authors: Gary Razinskas1, Robert Schindhelm1, Kathrin Breuer1, Stefan Weick1, Jörg Tamihardja1, Sonja Wegener1
1University Hospital Wuerzburg, Department of Radiation Oncology, Wuerzburg, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
On-couch adaptive radiotherapy provides the ability to alter treatment plans on a daily basis to account for interfractional anatomical variations. The AI-driven Varian Ethos solution is able to deliver personalized patient care based on daily cone-beam computed tomography (CBCT) images. Artifacts and uncertainties in Hounsfield Units (HU) due to photon scattering are known limitations of this imaging modality making its use for direct dose calculation challenging. To this end, a synthetic CT (sCT) is utilized by employing a CBCT-based deformable image registration of the planning CT (pCT) with its high image quality and calibrated density data. Since the accuracy of this sCT plays a key role in plan optimization and dose calculation, a comparison of sCT and CBCT is essential to detect potential errors.
Material and Methods
The first treatment sessions of each of our first 25 adaptive treatment plans at the Ethos were imported into the Eclipse treatment planning system (version 15.6). All adaptive treatments were performed in the pelvic region (10x cervix, 8x rectum, 7x prostate). The dose distributions of the adapted plans were retrospectively recalculated on the CBCT recorded prior the adaptation process using the AcurosXB algorithm. For this purpose, a reliable CBCT-HU calibration curve was implemented for the utilized pelvis preset considering patient group specific calibration data established on Ethos. CBCT- and sCT-based dose distributions where compared with regard to characteristic DVH metrics for target and organ at risk (OAR) structures.
Results
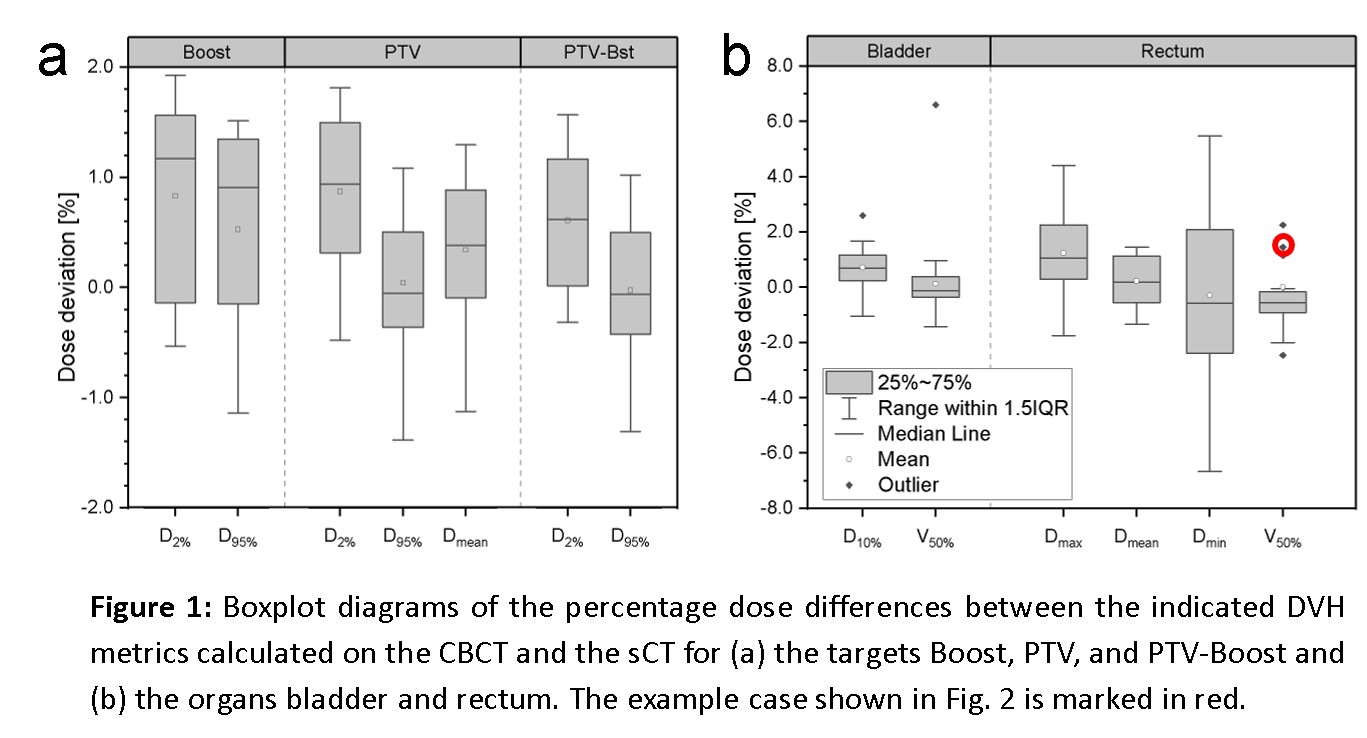
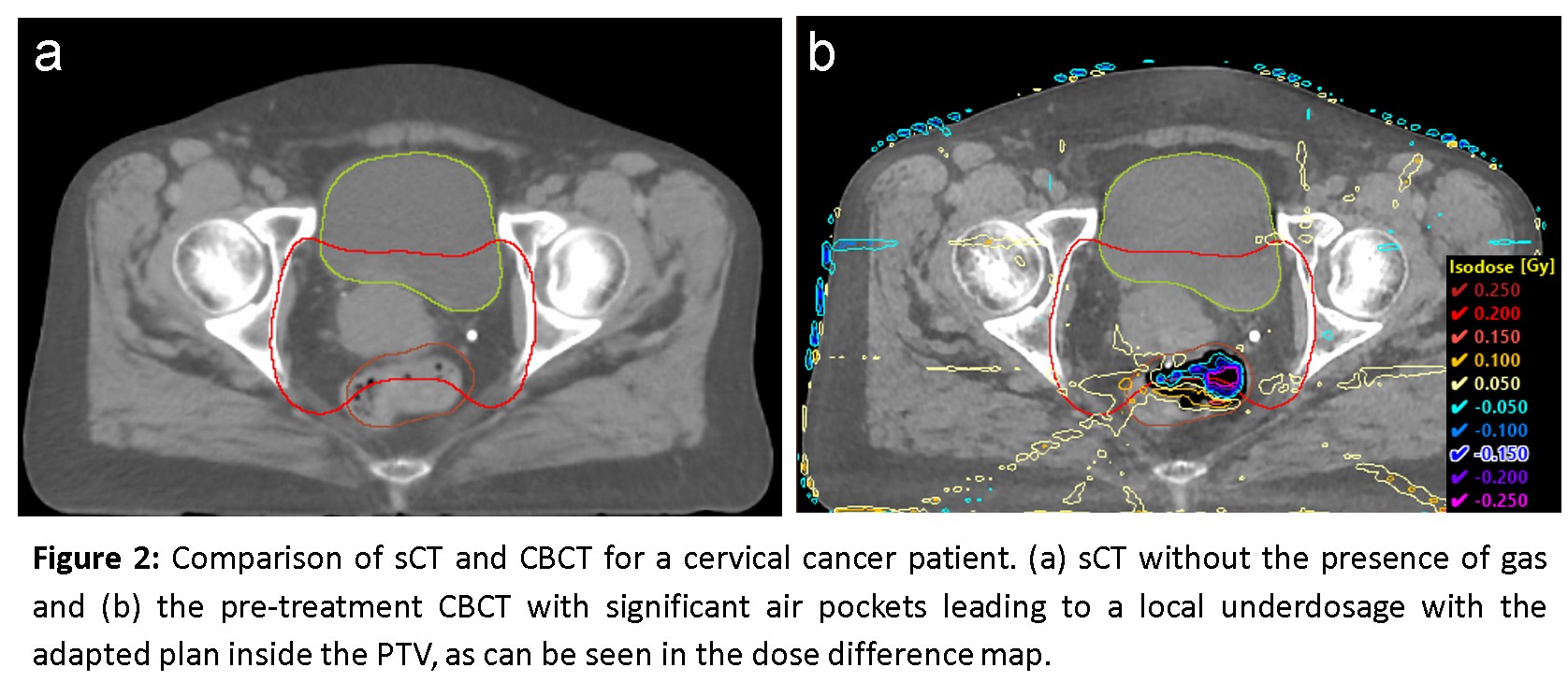
In the pelvic region, dose recalculation on the Ethos CBCT yielded excellent agreement in target coverage (Dmean, D2%, D95%) of PTV and Boost (Fig. 1a), with mean deviations below 1%. Dose deviations for relevant OAR parameters were also well below 2.5%, except for minimum and maximum doses (Fig. 1b). Furthermore, we encountered significant local deviations attributed to non-reproducible air pockets solely present during the adaptation. Figure 2 shows a cervical cancer patient’s sCT with no gas present (Fig. 2a) and the pre-treatment CBCT with significant air pockets leading to a local underdosage with the adapted plan inside the PTV (Fig. 2b) by 10% of the fraction dose (2 Gy).
Conclusion
CBCT-based dose calculation provides an efficient QA tool to detect situations where the sCT does not adequately represent the anatomy of the day, resulting in inaccurate dose calculations. Quality assessment of the sCT complements the standard secondary dose calculation performed before adaptive treatment. In the short term, this procedure can assist in safely expanding the adaptive treatment to sites beyond the pelvis with large density differences and geometrical changes, e.g. head-and-neck and lung. In longer term, direct dose optimization and calculation on the CBCT instead of the sCT could allow adaptation despite major anatomical changes and deformation algorithms reaching their limits.