Dosimetry predictors for haematological toxicity in chemoradiotherapy for cervical cancer
Mohammed Abdul-Latif,
United Kingdom
PO-1410
Abstract
Dosimetry predictors for haematological toxicity in chemoradiotherapy for cervical cancer
Authors: Mohammed Abdul-Latif1, Jananie Perera1, Hannah Tharmalingam1, Yatman Tsang1, Peter Hoskin2,1
1Mount Vernon Cancer Centre, Clinical Oncology, Northwood, United Kingdom; 2University of Manchester, Division of Cancer Sciences, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Concurrent chemoradiotherapy (CRT) with weekly cisplatin followed by image-guided brachytherapy is the standard of care for locally advanced cervical cancer (LACC). Haematological toxicity (HT) is a significant side effect, leading to interruptions in treatment, dose reductions or chemotherapy omission. Half of active bone marrow lies within the lumbar sacral spine (LS), pelvic bones (PB) and proximal femurs – much of which is inevitably irradiated during treatment.
This study aims to investigate the relationship between dosimetry of different irradiated bone regions and HT experienced by patients undergoing radical chemoradiotherapy for LACC.
Material and Methods
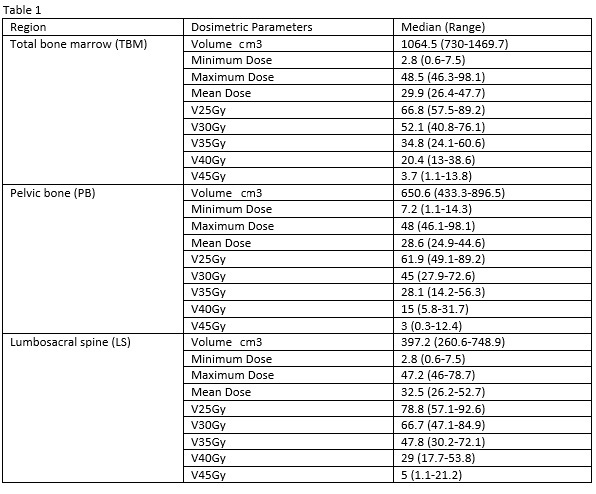
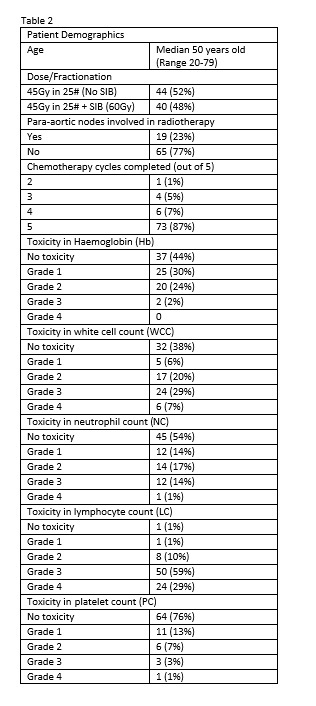
A retrospective review of patients with LACC who received radical CRT with or without simultaneous integrated boost (SIB at 60Gy) to positive lymph nodes and high-dose rate brachytherapy was conducted. Full blood counts at end of CRT were reviewed to collate haemoglobin (Hb), white cell count (WCC), neutrophil count (NC), lymphocyte count (LC) and platelet count (PC). HT was graded as per CTCAE version 5.0 criteria. Dosimetric data as shown in table 1 for LS (Lumbar spine up to 2cm above PTV in addition to sacrum), PB (Pelvic bones excluding LS and femoral heads) and total bone marrow (TBM – a combination of LS and PB) was recorded. Clinical demographic and dosimetric data were analysed for correlation with risk of HT using univariate and multiple logistic regression models.
Results
Between 2015-2021, eighty-four patients who had received radical CRT for LACC were included in this study.
The incidence of ≥grade 3 toxicity in Hb, WCC, NC, LC and PC were 26%, 36%, 15%, 88% and 5% respectively.
Multiple logistic regression analysis demonstrated PB V45Gy with HR of 1.2 (95% CI 1.0-1.4), LS V40Gy with HR of 1.1 (95% CI 1.0-1.2), PB minimum dose with HR of 1.3 (95% CI 1.0-1.6) were independent factors (p<0.05) in the development of ≥grade 2 Hb, WCC and PC toxicity respectively. LS maximum dose was associated with grade 4 LC toxicity with HR of 1.1 (95% CI 1.0-1.2).
No statistically significant factors were identified to correlate with risk of ≥grade 2 NC.
Conclusion
This study suggested that dose-volume parameters for LS and PB were statistically correlated to the risk of developing HT in patients receiving LACC CRT, although the effect was small. The number of chemotherapy cycles, the presence of SIB and the inclusion of para-aortic nodes in RT did not impact on the development of HT.