The most common histopathological type was ESS (49/81, 60.4%), followed by LMS (32/81, 39.6%). The median age at diagnosis was 50 years for LMS and 41 years for ESS. A total of 80 (98.7%) patients (31 for LMS and 49 for ESS) underwent surgery. Eighteen (56.2%) patients were early stage (FIGO stage 1& 2), 14 (43.75%) were advanced stage (3 & 4) for LMS. Thirty (61.1%) patients were early stage & 14 (28.6%) were in the advanced stage of ESS. Twelve patients (37.5%) for LMS and 9 (18.3) for ESS had positive surgical margins. In the case of LMS, ten patients (31.3%) received adjuvant External Beam Radiation (EBRT), and 17 (53%) received chemotherapy (Table1). In the case of ESS, 20 patients (40.8%) received pelvic EBRT, and 14 (28.5%) received chemotherapy. The most common pattern of failure for LMS was distant relapse (21, 65.6%) followed by local relapse (8, 25%), and for ESS, eight patients (16.3%) had a distant relapse, and 7 (14.2%) had a loco-regional relapse. Median overall survival (OS) was 19 months, progression-free survival (PFS) was 11 months, 2-year OS was 45.9%, and 2-year PFS was 34.6% for LMS. In the case of ESS, 2-year OS was 83%, and 2-year PFS was 76% (Figure1). The tumor stage (p=0.02), size of the tumor (p=0.02) for LMS and Low grade (p=0.03), and positive margins (p=0.01) for ESS were significantly associated with PFS.
Table1: Patient and Treatment characteristics of Uterine Sarcomas
Patient & treatment characteristics
| LMS (n=32)
| ESS (n=49)
|
Median age (Range)
| 50 years
(36-72 years)
| 41 years
(20-71 years)
|
Menopause attained
| 16 (50%)
| 15 (30.6%)
|
FIGO stage
1&2
3&4
|
18(56.25%) 14(43.75%)
|
30(61.1%) 19(38.9%)
|
Grade
Low-grade ESS
High-grade ESS
|
|
27(55%) 22(45%)
|
Primary surgery
| 31(96.9)
| 49(100%)
|
Positive surgical margin
| 12 (37.5%)
| 9(18.3%)
|
Pelvic EBRT
| 10(31.3)
| 20 (40.8%)
|
Chemotherapy
| 17(53.1%)
| 14 (28.5%)
|
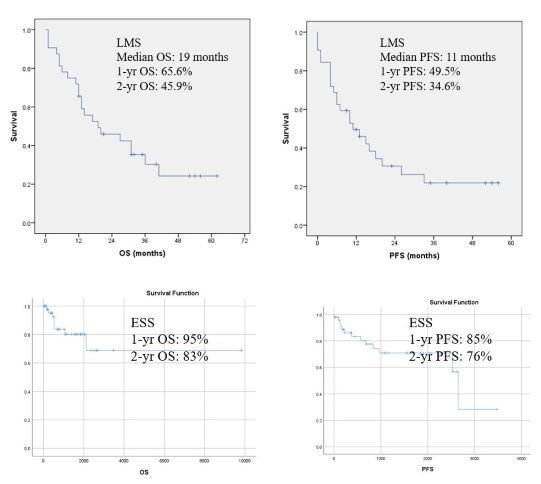 Figure1: Survival curves for PFS and OS
Figure1: Survival curves for PFS and OS