Effectiveness and safety of Hypofractionated Stereotactic Radiotherapy in pituitary adenomas
Virginie Delgrange,
France
PO-1139
Abstract
Effectiveness and safety of Hypofractionated Stereotactic Radiotherapy in pituitary adenomas
Authors: Virginie Delgrange1, Caroline Beaudelot2, Laetitia Padovani3, Nicolas Deleval4, Etienne Marchal5, Robin Fabbro6, Adrien Laville6, Alexandre Coutte6, Michel Lefranc7
1University Hospital Amiens, Radiotherapy, Amiens, France; 2Oscar Lambret Center, Radiotherapy, Lille, France; 3University Hospital of Marseille La Timone, Radiotherapy, Marseille, France; 4University Hospital of Amiens, Radiology, Amiens, France; 5University Hospital of Amiens, Nuclear Medicine , Amiens, France; 6University Hospital of Amiens, Radiotherapy, Amiens, France; 7University Hospital of Amiens, Neurosurgery, Amiens, France
Show Affiliations
Hide Affiliations
Purpose or Objective
Pituitary adenomas (PA) are mostly treated by surgery or medical treatment.
Radiation therapy is indicated as a treatment for residual or recurrent pituitary adenomas after surgery, in order to reduce hormonal or visual symptoms related to the adenoma progression.
Conventional radiation therapy (CRT) is indicated for tumors of any and Radiosurgery (SRS) is mainly indicated for PA <3cm and located more than 2mm away for the optic pathways. The role of hypofractionated stereotactic radiotherapy (HFSRT) for the treatment of these tumors is unclear.
The aim of this study is to compare HFSRT to CRT in terms of efficacy (local control, hormonal normalization, visual control) and safety (toxicities, visual deterioration, new hypopituitarism).
Material and Methods
We retrospectively analyzed data from patients treated with radiotherapy for pituitary adenoma at the University Hospital of Amiens and Marseille between 2011 and 2020. 38 patients were treated with HFSRT with the Cyberknife, and 38 patients were treated with CRT with Intensity Modulated Radiotherapy.
For HFSRT, 3 x7 Gy, or 5x5 Gy were prescribed for nonfunctioning adenomas whereas 3 x10-12 Gy for secretory adenomas. For CRT, 26 to 30 fractions of 1,8-2 Gy were used.
Results
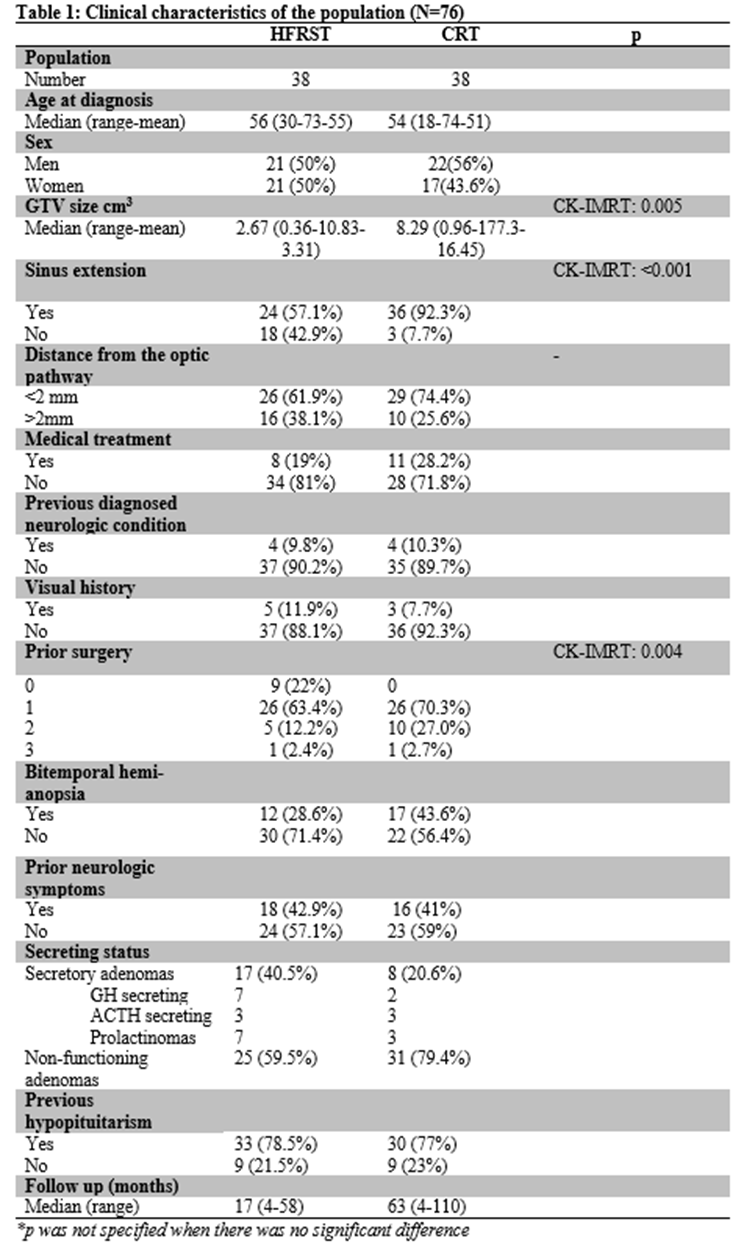
The clinical characteristics of the population are shown in the table 1.
For HFRST, the median mean dose to the GTV was 32.27 Gy (19.82-50.76), with a median prescription isodose of 56.4 % (48.6-68), and a median gradient of 2.81(2.45-4).
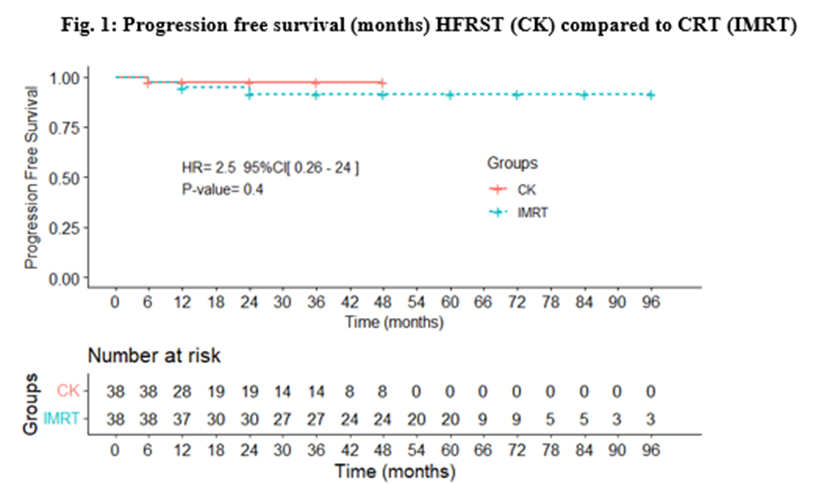
Patients at the HFSRT group achieved a local control rate (LCR) of 100% at 1 and at 2 years, whereas those who received CRT achieved LCR of 100% and 97% at1 and at 2 years, respectively.
Progression-free survival (PFS) was not significantly different between the two techniques (HR=2. 5, 95%CI (0. 26-24), p=0.4).
In the multivariate analysis, there were no significant correlations between the independent variables (dose, number of surgeries before radiotherapy, sinus extension, GTV size and secretory status) and local control at 1 year, and two years.
Time to hormonal normalization was not significantly different (HR 0. 59 CI 95% (0. 25-1. 4), p=0. 24) between groups.
For the subgroup of adenomas close to the optic tract (<2mm), there was no more visual deterioration or visual improvment with HFSRT compared to CRT, at 1 year (p=0,73), 2 years (p=0,99), and 3 years (p=0,89).
Toxicity rates were low, and there was no significant difference between the two techniques regarding the incidence of hypopituitarism (p=0. 68).
Conclusion
Compared to conventional radiotherapy, hypofractionated stereotactic radiotherapy allows a similar rate of local control and hormonal normalization without generating a higher rate of hypopituitarism. It can be used as an alternative for peri-optic and < 3cm3 adenomas. However, additional studies are needed for larger adenomas