Ultrasound is preferable to MRI as imaging modality during high frequency mechanical ventilation
Irma van Dijk,
The Netherlands
PO-1894
Abstract
Ultrasound is preferable to MRI as imaging modality during high frequency mechanical ventilation
Authors: Jeffrey Veldman1, Zdenko van Kesteren1, Michael Parkes1, Markus Stevens2, Joost van Schuppen3, Joost van den Aardweg4, Geertjan van Tienhoven1, Arjan Bel1, Irma van Dijk1
1Amsterdam UMC - location University of Amsterdam, Department of Radiation Oncology, Amsterdam, The Netherlands; 2Amsterdam UMC - location University of Amsterdam, Department of Anaesthesiology, Amsterdam, The Netherlands; 3Amsterdam UMC - location University of Amsterdam, Department of Radiology, Amsterdam, The Netherlands; 4Amsterdam UMC - location University of Amsterdam, Department of Pulmonology, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Respiratory motion management (RMM) in radiotherapy is recommended for tumours that move more than 5 mm due to breathing. During free breathing, large PTVs or ITVs are defined to account for respiratory motion, leading to unnecessary dose to healthy tissue. Reducing motion amplitude using mechanical ventilation may lead to reduction in target volumes. In our study, we quantify the effect of several breathing control strategies on organ and diaphragm motion, mainly measured on MRI. However, MRI is expensive and may be cumbersome for subjects. Alternatively, ultrasound (US) is more available and has a higher temporal resolution but may be more variable due to intra-operator variation. Our purpose was to determine if US is as accurate as MRI to quantify diaphragm motion during non-invasive mechanical ventilation at 60 breaths per minute (brpm).
Material and Methods
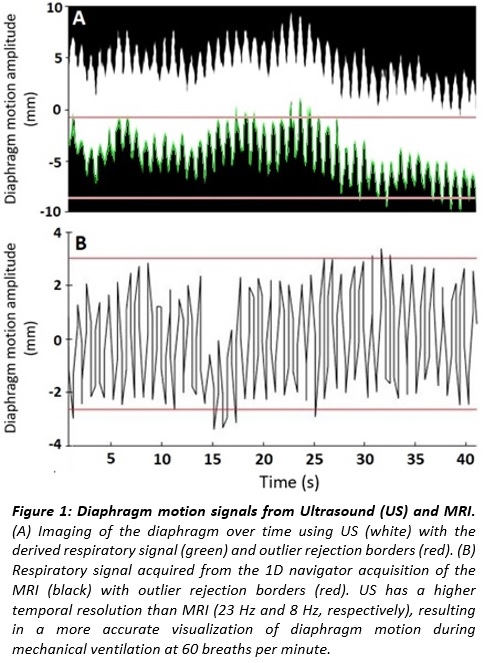
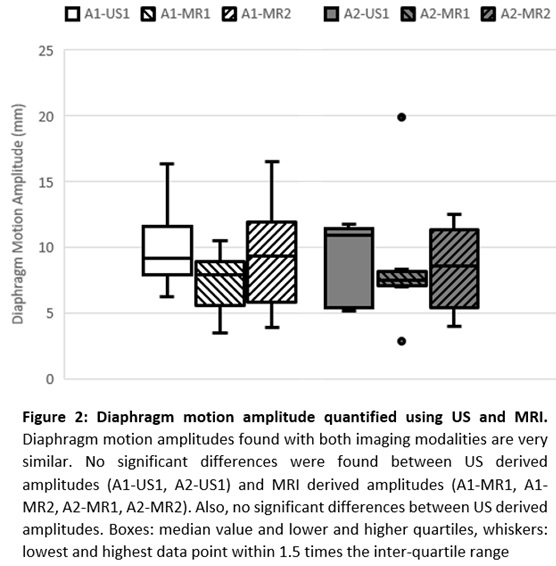
After ethics committee approval and written informed consent, six healthy volunteers enrolled and practiced being non-invasively ventilated at 60 brpm. In one subsequent session, diaphragm motion amplitude (A) was measured twice for 40 seconds using US cine-imaging (A1-US1 and A2-US1). We selected a sagittal plane on the mid-clavicular line and determined diaphragm motion amplitude on a point 10 cm from the imaging probe with a temporal resolution of 23 Hz. In two MRI sessions, on separate days, diaphragm motion amplitude was measured twice for 40 seconds (A1-MR1, A2-MR1, A1-MR2, A2-MR2) using a 1D navigator acquisition at 8 Hz, placed on the liver top at the level of the pancreas in anterior-posterior direction. From all 40 s measurements, we acquired diaphragm motion over time, to which we applied 5% outlier rejection (excluding 5% of the data points whilst minimizing the amplitude), resulting in an amplitude representative for the diaphragm motion amplitude imposed by the ventilation (Figure 1). We compared the first 40 seconds of each session (A1-US1, A1-MR1 and A1-MR2) and the second 40 seconds (A2-US1, A2-MR1 and A2-MR2) We used paired Wilcoxon’s test to test for significant differences (p<0.05). Additionally, we quantified the difference between A1-US1 and A2-US1, to identify any intra-operator variation.
Results
Median diaphragm motion amplitudes A1 were 9.1 mm, 7.9 mm and 9.4 mm on US1, MR1 and MR2 respectively. Median amplitudes A2 were 10.9 mm, 7.5 mm, and 8.6 mm, respectively (Figure 2). Median diaphragm motion amplitudes were not significantly different between the US derived amplitudes and MRI derived amplitudes (0.12<p<0.90). There was also no significant difference between A1-US1 and A2-US1 (p=0.36), indicating that there was no apparent intra-operator variation.
Conclusion
Ultrasound is as equally accurate as MRI to quantify diaphragm motion during mechanical ventilation at 60 brpm, and preferred over MRI due to its availability, lower costs and higher temporal resolution.