Dosimetric impact of intrafraction motion for prostate SBRT with dose escalation on the index-tumor
Marie-Claude BISTON,
France
PO-1882
Abstract
Dosimetric impact of intrafraction motion for prostate SBRT with dose escalation on the index-tumor
Authors: Marie-Claude BISTON1, Francesca DI FRANCO1, Anne-Agathe SERRE1, Thomas BAUDIER1, Olivier ROUVIERE2, Vanina ISNARDI3, Pascal POMMIER4
1Centre Leon Berard, Radiotherapy department, Lyon, France; 2Hospices Civils de Lyon, Department of Urinary and Vascular Imaging, Lyon, France; 3Centre Leon Berard, Nuclear Medicine department, Lyon, France; 4Institut de cancérologie de l'Ouest Paul-Papin, Radiotherapy department, Angers, France
Show Affiliations
Hide Affiliations
Purpose or Objective
The feasibility of dose escalation (>95GyEQD2) on the index tumor (IT) using SBRT was showed to increase the therapeutic ratio for patients with localized prostate cancer. In this case, it is important to minimize daily pelvic anatomical changes and prostate intrafraction motion, under penalty of increasing the treatment toxicity. The objective was to evaluate the dosimetric impact of both daily anatomical variations alone, and in combination with prostate intrafraction motion, on the 2 first patients irradiated with such protocol within the framework of a multicenter trial.
Material and Methods
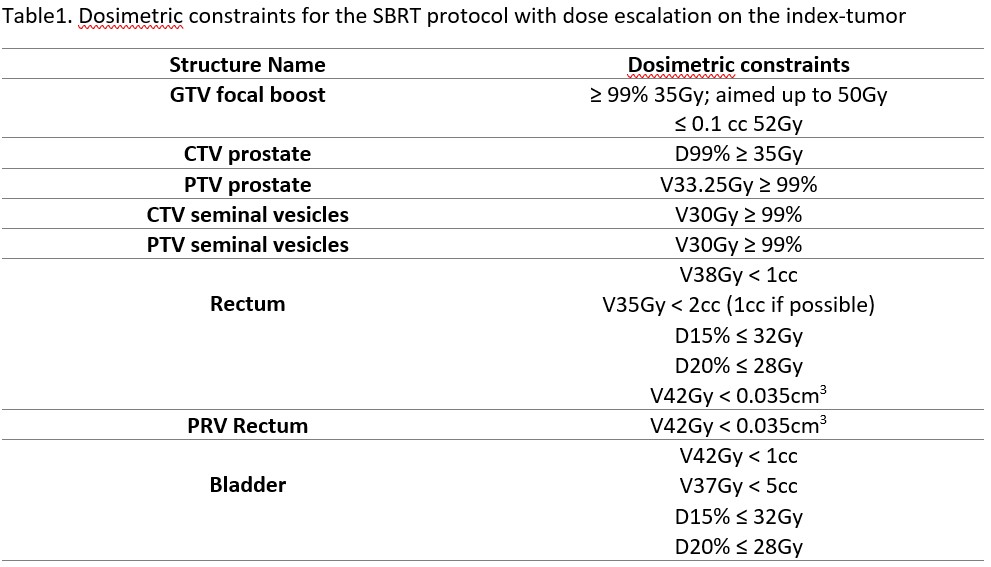
For the two patients (P1, P2), the delineation of the IT was based on the combination of multi-parametric MRI and 68Ga-PSMA PET. The prescription dose was 35Gy in 5 fractions delivered to the clinical target volume (CTV) using VMAT technique. The main dosimetric objectives are listed in Table 1. CTV-to-Planning Target Volume (PTV) margins were 5mm. Pre-treatment positioning and intrafraction motion monitoring were performed using daily Cone Beam CT (CBCT) imaging and a transperineal ultrasound probe, respectively. For performing dose accumulation (accumulated CT, aCT), Planning CT (pCT) images were deformably registered onto daily CBCT using ADMIRE V3.37 (Elekta AB, Stockholm) software to generate synthetic CT (syCT). The beam were split in sub-arcs which were thereafter synchronized with registered prostate motion. The dose calculation was finally performed using the voxel shifting method. The shifted dose maps were finally accumulated (moved-accumulated CT, maCT).
Results
No significant change in CTV volumes delineated on daily syCT compared to pCT was observed. Regarding GTV coverage, D99% decreased from 38.8Gy and 40.2Gy on pCT to 36Gy and 37.7Gy on aCT, and 35.4Gy and 35Gy on maCT, for P1 and P2, respectively. A loss of CTV coverage (≥5%) was also observed for the 2 patients only on the maCT. PTVcoverage was decreased by up to 3.6% on aCT and up to 18.6% on maCT. The rectum was smaller than planned in 50% of fractions but the dosimetric differences were not significant with the exception of D15% for P2 which was found significantly smaller on the maCT (24.7Gy) than on the pCT (30.1Gy). The bladder was smaller than planned in 60% of fractions. On average the differences were smaller than 2Gy between the pCT and aCT. Conversely, significant differences were found (> 3.3Gy and up to 5.9Gy) between the pCT and maCT. Finally the V37Gy was significantly impacted for P1, going from 0.6cc on the pCT to 4cc on the maCT, but the dosimetric constraints were respected.
Conclusion
The dosimetric effect of prostate intrafraction motion on targets’ coverage and organs at risk was shown to predominate over anatomical variations alone. Further investigations are in progress to evaluate the impact of the interoperator variability in the IT contouring and treatment planning on the dose distribution.