Individual monitoring of dosimetric changes in head and neck adaptive proton therapy
PO-1860
Abstract
Individual monitoring of dosimetric changes in head and neck adaptive proton therapy
Authors: Ana Turkaj1, Benedetta Siniscalchi1, Irene Giacomelli2, Mattia Bertolini1, Mirco Lipparini1, Luca Pomino3, Annalisa Trianni4, Paolo Farace3, Marco Cianchetti3
1Proton Therapy Unit and Medical Physics Department , Azienda Provinciale per i Servizi Sanitari, Trento, Italy; 2Proton Therapy Unit and Medical Physics Department , Azienda Provinciale per i Servizi Sanitari, Trento, Italy; 3Proton Therapy Unit and Medical Physics Department, Azienda Provinciale per i Servizi Sanitari, Trento, Italy; 4Medical Physics Department , Azienda Provinciale per i Servizi Sanitari, Trento, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Proton Therapy (PT) is sensitive to anatomical changes that may distort the planned dose distribution and impact the treatment quality. In non-adaptive treatment, robust anatomical planning on approximate modeling might manage some anatomical changes with a potential decrease in plan quality. Adaptive strategies are recommendable, but they are technically and resource-demanding. Few studies reported the impact of individual monitoring of dosimetric changes occurring over PT treatment, and more data are required to drive the development of optimal adaptive strategies. In this study, we retrospectively evaluated head and neck (HN) patients treated for four years in our center, presenting the advanced workflow, based on monitoring by repeated computer tomography (CT) scans, implemented during the study.
Material and Methods
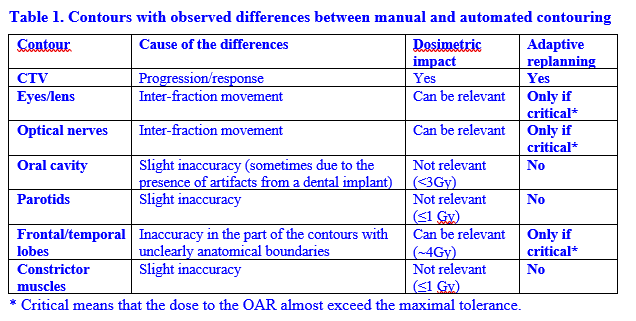
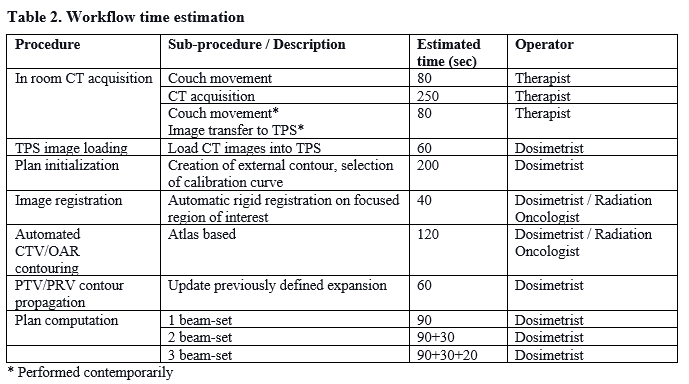
Repeated CT scanning was performed on 201 patients to recognize dynamic anatomical changes during HN PT. The image-driven workflow we implemented includes in-room CT on-rails for image acquisition, automatic contouring using planning CT as atlas data, and fast dose computation on a Graphics Processing Unit by a Monte Carlo algorithm. Quality assurance (QA) of the automatic contouring was performed on seven patients (three with slimming and four with target modifications) by comparison with manual contouring to verify the reliability of that automated process and the eventual necessity of medical supervision. The time duration to perform each phase of the workflow was assessed. Finally, we calculated the number of patients who required replanning, identifying the causes for such an adaptive modification.
Results
Contours QA (Table 1) showed differences between the manual and automated process in only a few organs at risk (OAR), with dose differences in even fewer cases. Manual correction for accurate evaluation is not indispensable when the dose to the OAR is far from tolerance limits. The target needs always to be verified to identify progression/response. Table 2 reports the estimated time required to perform every workflow phase, with a total time of approximately 16-17 mins. Sixteen of the treated patients required treatment replanning for different reasons: variation in the cavity filling, weight loss and slimming, change in the target volume, and consequent target under-dosage.
Conclusion
Start-of-the-art technology is mature for an affordable and time-efficient workflow, mostly automatized, for repeated CT acquisition, contouring, and dose computation. Our data showed that anatomical changes, which required adaptive replanning, typically occur in only a small number of patients (8 % of cases in our sample of more than two hundred patients). The reasons for replanning are different, and it would be hard to model all of them. In light of the above, individual monitoring by repeated CT scans to select patients who require treatment replanning seems an optimal strategy in adaptive HN PT.