Investigating the use of Microsoft KinectV2 to monitor a patient’s breathing during Lung SBRT
Gail Anastasi,
United Kingdom
PO-1845
Abstract
Investigating the use of Microsoft KinectV2 to monitor a patient’s breathing during Lung SBRT
Authors: Gail Anastasi1,2, Philip Evans2, Elizabeth Adams1, Catharine Clark3, Kevin Wells2, Andrew Nisbet4, Veni Ezhil5
1Royal Surrey Hospital Foundation Trust, Radiotherapy Physics, Guildford, United Kingdom; 2University of Surrey, Centre for Vision, Speech and Signal Processing, Guildford, United Kingdom; 3University College London Hospitals NHS Foundation Trust, Radiotherapy Physics, London, United Kingdom; 4University College London, Medical Physics and Biomedical Engineering, London, United Kingdom; 5Royal Surrey Hospital Foundation Trust, Clinical Oncology, Guildford, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
To determine whether a KinectV2 camera can be used to monitor the variation in breathing trace via chest surface motion during Lung SBRT treatments.
Material and Methods
Ten lung SBRT patients were recruited to a study where breathing traces (at 4DCT and each of 3, 5 or 8 treatment fractions) were acquired. At 4DCT and 4DCBCT (preceding the 1st fraction) a trace was acquired via 2 external imaging devices as surrogates for internal tumour motion: the Varian Respiratory Gating for Scanners (RGSC) system and KinectV2 (attached to the Couch at CT and to a ceiling mount in the Linac room). A region of interest (LT or RT of the RGSC block) on the patients’ chest surface was selected from the KinectV2 surface images. The average depth to this ROI was calculated and compared to the RGSC trace. For the treatment delivery only KinectV2 was employed. Lung SBRT was delivered with a 2 Arc VMAT plan, and KinectV2 acquisitions performed for both Arcs. A mean breathing cycle was calculated from the whole trace acquired during the time to deliver each Arc. This was performed by identifying peaks in each trace, splitting into individual cycles and finally binning these into 10 phases.
Results
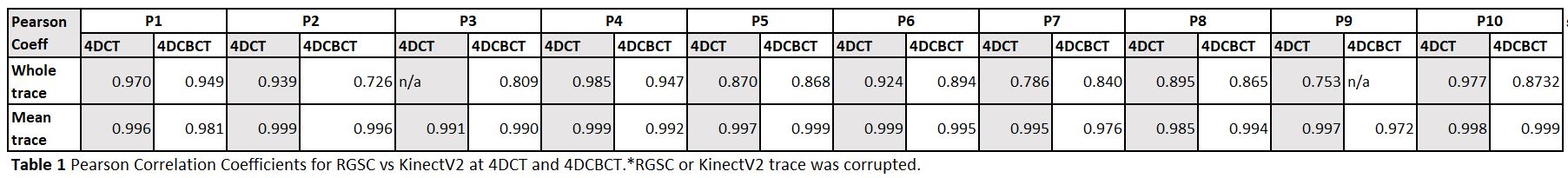
The absolute amplitude of the RGSC and KinectV2 traces are not directly comparable. The KinectV2 gives a line of sight depth map in the ROI as opposed to the Ant/Post motion perpendicular to couch given by the RGSC system. The KinectV2 signal exhibited low frequency variations as the couch moved into the bore at CT and as the gantry rotated during treatment, most likely due to change in the infra—red signal reflecting off the moving equipment and onto the selected ROI. There was very good agreement in phase over all 10 patients (see Table 1) with an average Pearson correlation coefficient for RGSC vs Kinect across both imaging modalities of 0.882±0.076 and 0.993±0.007 for the whole trace and mean breathing cycle, respectively.
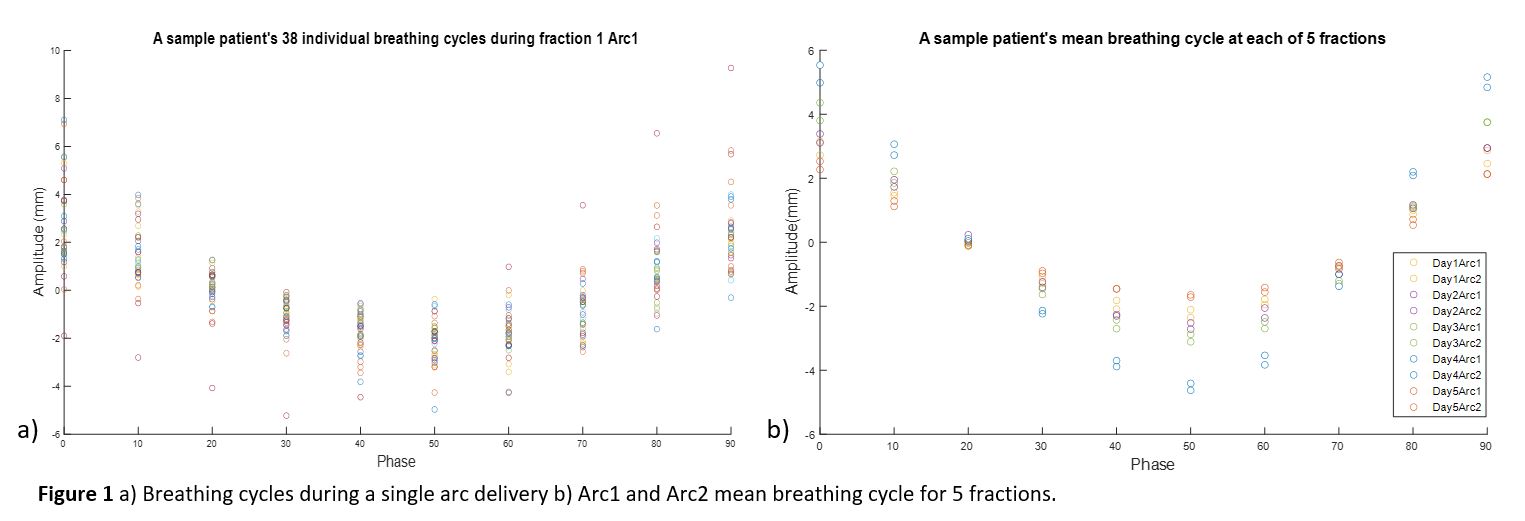
It was possible to perform KinectV2 acquisitions at treatment for all 10 patients, with no impact to patients or treatment session time. A similar pattern of variability in breathing traces was observed through treatment of all 10 patients. Figure 1a shows the variability in 38 individual breathing cycles making up the entire trace acquired from KinectV2 during delivery of fraction1 Arc1 for a sample patient. The mean standard deviation across all phases was ± 2.4mm. Figure 1b shows the variability in the mean breathing cycle (eg Day1Arc1 is the mean cycle from Figure 1a) acquired during Arcs 1 and 2 across the 5 fractions for the same patient. The mean standard deviation across all phases was ± 0.7mm.
Conclusion
There exists a strong correlation between traces obtained from the KinectV2 and RGSC system. KinectV2 can be used in a clinical setting to measure variability in chest surface motion through a patient's lung SBRT treatment. Monitoring the trace will give the confidence required to reduce target volumes by applying personalised margins based on variability due to breathing.