Simple AP/PA techniques to deliver total skin electron beam therapy to frail patient while recumbent
PO-1792
Abstract
Simple AP/PA techniques to deliver total skin electron beam therapy to frail patient while recumbent
Authors: Xin Wang1, Ramesh Tailor1, Tze Yee Lim1, Bouthaina Shabib Dabaja2, Jillian Gunther2, Travis Rougeau3, Chelsea Pinnix2, Penny Fang2, Susan Wu2, Congjun Wang1
1MD Anderson Cancer Center, Radiation Physics, Houston, USA; 2MD Anderson Cancer Center, Radiation Oncology, Houston, USA; 3MD Anderson Cancer Center, Radiation Therapy, Houston, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
The delivery of total skin electron beam therapy (TSEBT) to frail patients unable to stand for long periods can be challenging. Complicated floor techniques were developed and used in our institution. Here, we present three simple and efficient techniques that allow delivery of TSEBT to patients while on a stretcher and compare the dosimetry of each method.
Material and Methods
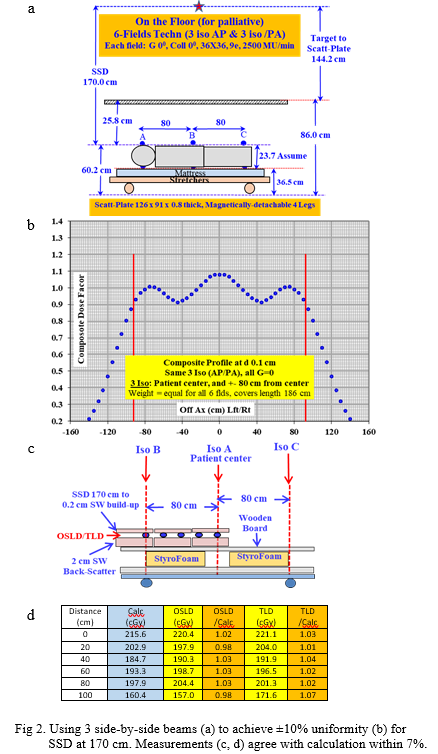
We compared three recumbent TSEBT approaches each using AP/PA beams. Two approaches utilize a gantry at 0 degree with the patient on a stretcher in the supine and prone position with an SSD of 170 cm (stretcher lowered to the floor) or an SSD of 186 cm (stretcher disassembled). The third approach utilizes a gantry position of 90 degrees with the patient in the lateral decubitus position at an SSD of 300 cm.
For all techniques, TSEBT is delivered on a Varian TrueBeam linac, interlocked to 9 MeV HDTSe mode with a jaw opening of 36x36 cm by a plate inserted into the accessory slot. A stack of aluminum and polymethyl methacrylate (PMMA), 0.584 and 5.918 mm in thickness, respectively, is mounted on the plate as a custom flattening filter and energy degrader. A spoiler made of 8 mm PMMA is used at ~25 cm from the patient’s surface.
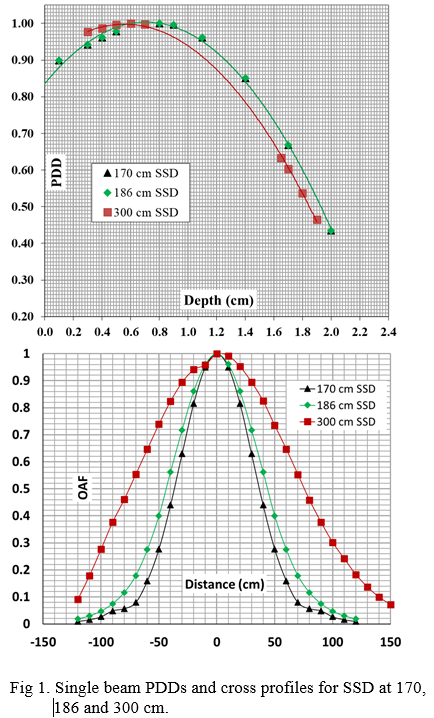
We performed single beam measurements with SSDs at 170, 186 and 300 cm. The measurements included PDD, cross profile and output. The cross profile were used to fit composite dose of adjacent beams with a goal of achieving ±10% dose uniformity. We opted for equal beam weighting and beam center markings on the stretcher to minimize the chance of error and treatment time. The optimal longitudinal separation between beams and the required MUs/beam were calculated. OSLD and TLD measurements in phantom at 3 mm depth were performed to verify the calculations.
Results
For both 170 and 186 cm SSD, PDD measurements showed 8 mm dmax, 1.95 cm R50 and 2.32 cm Rp. At 300 cm SSD, PDD showed 6 mm dmax, 1.85 cm R50 and 2.26 cm Rp. The cross profile measurement for 170 cm SSD had 30 cm width at 90% relative dose. Using 3 beams, equal weighting and a separation of 80 cm between adjacent beam centers, a uniformity of ±10% can be achieved within a distance of ~190 cm. At 186 cm SSD, a longer distance of 200 cm with ±10% uniformity can be achieved using 90 cm beam center separations. OSLD and TLD measurements agreed with the calculation to within 7%. 300 cm SSD widens the cross profile significantly with the 90% width reaching 60 cm. 2 junction beams with 160 cm separation were enough to achieve uniformity of ±6% over a 200 cm distance.
Conclusion
We developed three simple AP/PA techniques to treat frail TSEBT patients in the recumbent position. While 300 cm SSD supports better uniformity laterally, there may be advantages to the supine/prone positioning with the SSD=170 cm technique. These techniques are only intended for urgent treatments of a few fractions, as dosimetry is not ideal. The conventional standing technique should be used as soon as possible.