Effectiveness of Non-coplanar Monoisocenter Multifraction Radiosurgery for Multiple Brain Metastases
PO-2024
Abstract
Effectiveness of Non-coplanar Monoisocenter Multifraction Radiosurgery for Multiple Brain Metastases
Authors: Federico Colombo1, Francesco Salaroli2, Ilaria Renna2, Giovanni Ceccon2, Elisabetta Lattanzi2, Stella Gianni2, Claudia Grondelli2, Marialuisa Bergamini2, Cristina Dell'Anna2, Marco Galaverni2, Francesca Bozzetti3, Paolo Tortoli4, Michele Maddalo4, Aldo Mazzilli4, Giovanna Benecchi4, Caterina Ghetti4, Nunziata D'Abbiero2, Nicola Simoni2
1Azienda Ospedaliero Universitaria di Parma - Scuola di Specializzazione UNIMORE, Radiation Oncology Unit, Parma, Italy; 2Azienda Ospedaliero Universitaria di Parma, Radiation Oncology Unit, Parma, Italy; 3Azienda Ospedaliero Universitaria di Parma, Neuroradiology Unit, Parma, Italy; 4Azienda Ospedaliero Universitaria di Parma, Medical Physics Unit, Parma, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Synchronous irradiation of multiple brain metastases (mBMs) by means of Multifraction Stereotactic Radiosurgery (mfSRS) represents a challenge due to complex dose delivery process. Aim of the present study was to evaluate long-term outcomes of mfSRS for mBMs, using an innovative mono-isocenter non-coplanar technique.
Material and Methods
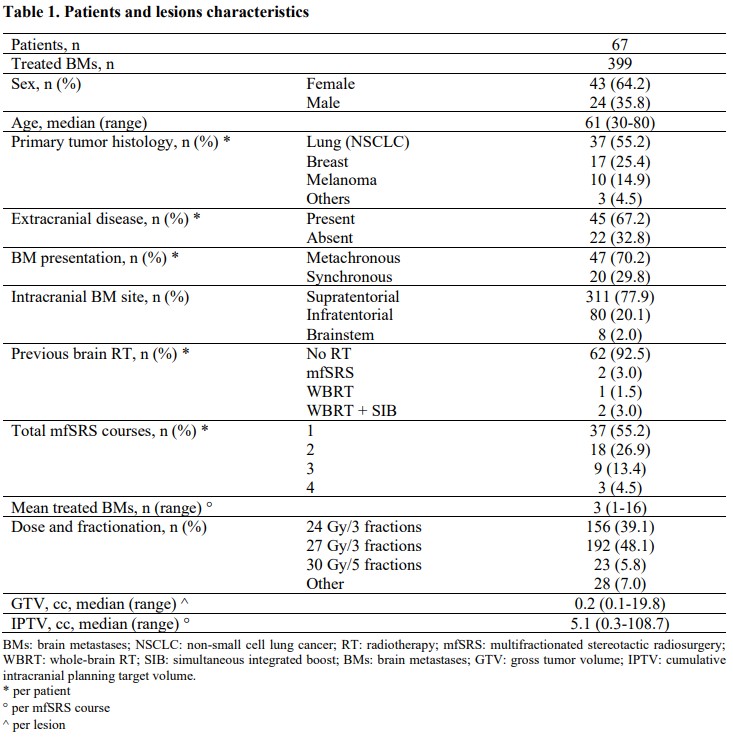
Patients with mBMs, good performance status (ECOG ≤ 2), and life expectancy > 3 months, treated with mfSRS from 2019 to 2021 at our Institution, were retrospectively evaluated. For radiotherapy planning, a mfSRS VMAT plan was generated with 5 non-coplanar arcs using HyperArc (Varian Medical System, Palo Alto, US). Primary endpoints were local progression-free survival (LPFS) and intracranial progression-free survival (iPFS).
Results
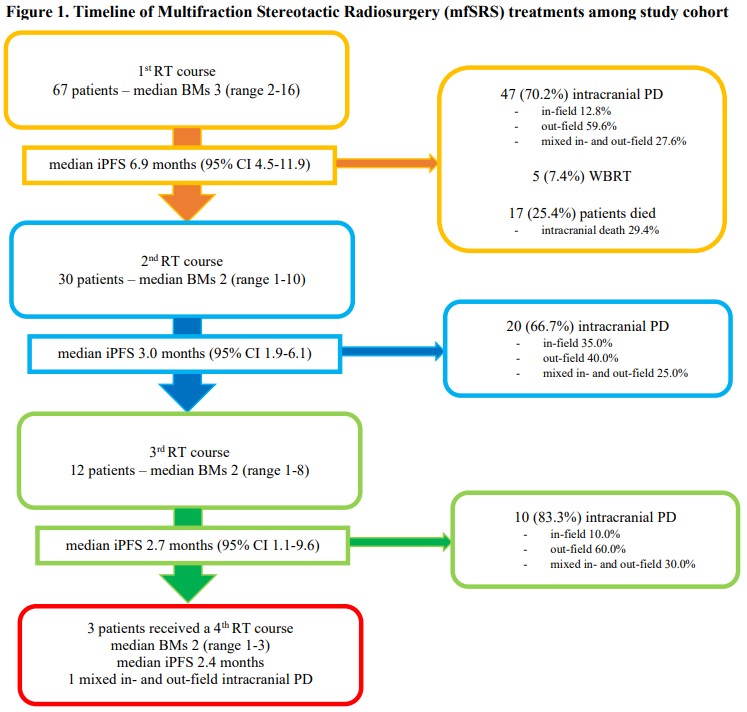
A total of 67 patients accounting for 399 brain metastases were analyzed. Non-small cell lung cancer (NSCLC) (55.2%), breast cancer (25.4%) and melanoma (14.9%) were the most frequent histologic types. The median number of treated metastases for mfSRS course was 3 (range 1-16), and the median lesion (GTV) and intracranial cumulative target volume (iPTV) were 0.2 cc (range 0.1-19.8) and 5.1 cc (range 0.3-108.7), respectively. With a median follow-up (FU) time of 10.5 months (range 0.8-36.4), the overall local control (LC) rate was 75.5%, with a 1- and 2-year LPFS of 72.2% and 65.6%, respectively. Median iPFS after first mfSRS course was 6.9 months (95% CI 4.5-11.9), and 30 (44.8%) patients received repeated mfSRS courses (range 2-4) for intracranial progression (IPD). Salvage whole-brain radiotherapy (WBRT) was used in 5 (7.4%) patients. At multivariate analysis, number of treated lesions (≥5) and histology (melanoma) correlated with LC and iPFS (HR 4.59 [95% CI 1.48-14.24]; p = 0.008 and HR 3.05 [95% CI 1.13-8.23]; p = 0.009) respectively. Radiological signs of radionecrosis or hemorrhage occurred in 1.6% of treated lesions; no other acute or late grade ≥3 toxicities were reported. The median overall survival (OS) of the entire cohort was not reached (95% CI 19.6 months-NE), with a 1- and 2-year OS of 76.7% and 60.7%, respectively.
Conclusion
Multifraction Stereotactic Radiosurgery with mono-isocenter non-coplanar technique represents an effective treatment option for selected patients with mBMs. Considering the high local control rate and the excellent toxicity profile, it appears to be an attractive approach compared with WBRT, especially in the context of a multimodal patient management.